The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
Overdose is more likely among patients who discharge themselves from hospital before medically advised
Khan M, Hu X, Crabtree A, Moe J, Nasmith T, Daly-Grafstein D, Brubacher JR, Slaunwhite AK, Staples JA. “Before medically advised” departure from hospital and subsequent drug overdose: a population-based cohort study. CMAJ. 2024;196(31):E1066-E1075.
While many inpatients wait for a physician to discharge them from hospital, some choose to discharge themselves before being medically advised (BMA), which can have negative health outcomes. Advancing Health Scientists Drs. John Staples and Amanda Slaunwhite compared the rate of illicit drug overdose in the 30-day period after a hospital stay among patients who chose BMA discharge versus physician-advised discharge. Of 189,808 analyzed hospital stays in B.C., 6,440 ended in BMA discharge. Compared with physician-advised discharge, patients who chose a BMA discharge were more likely to have a history of illicit drug and/or alcohol use, overdose, homelessness, and recent hospital admission for a psychiatric condition. A total of 820 overdoses occurred in the 30 days following hospital discharge, with overdose risk being 58% higher among patients who initiated BMA discharge compared with physician-advised discharge. These findings indicate that evidence-based protocols should be developed and implemented to discourage BMA discharge, where possible, and improve post-discharge outreach to reduce the risk of overdose.

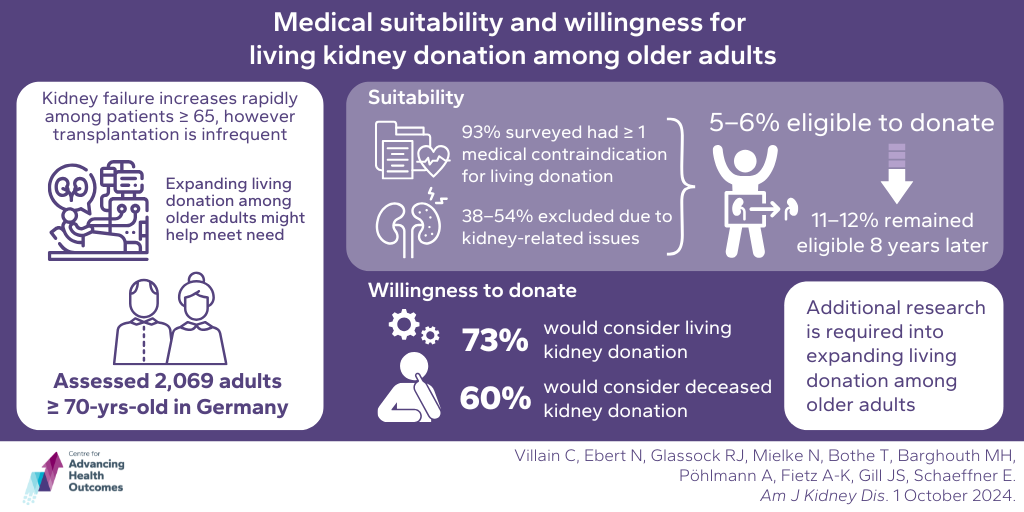
Many older adults are willing to be living kidney donors, but suitability could be an issue
Villain C, Ebert N, Glassock RJ, Mielke N, Bothe T, Barghouth MH, Pöhlmann A, Fietz A-K, Gill JS, Schaeffner E. Medical suitability and willingness for living kidney donation among older adults. Am J Kidney Dis. Published online October 1, 2024.
Researchers, including Advancing Health’s Dr. John Gill, analyzed data from 2,069 adults aged 70 years and over to determine the suitability and willingness of living kidney donation among older adults. Of the participants, 93% had at least one medical contraindication for living donation, plus 38–54% kidney-related issues. In all, 5–6% of the study population had neither medical nor kidney-related exclusions and were therefore eligible for living donation. Of these, only 11–12% were still eligible for living donation eight years later. While the suitability for living kidney donation was not overly high, willingness to donate was: 73% of participants would consider living kidney donation, while 60% would consider deceased kidney donation. Because of the mismatch between eligibility and willingness to donate, the team concluded that additional research is required to expand living donation among older adults and meet kidney transplantation needs.
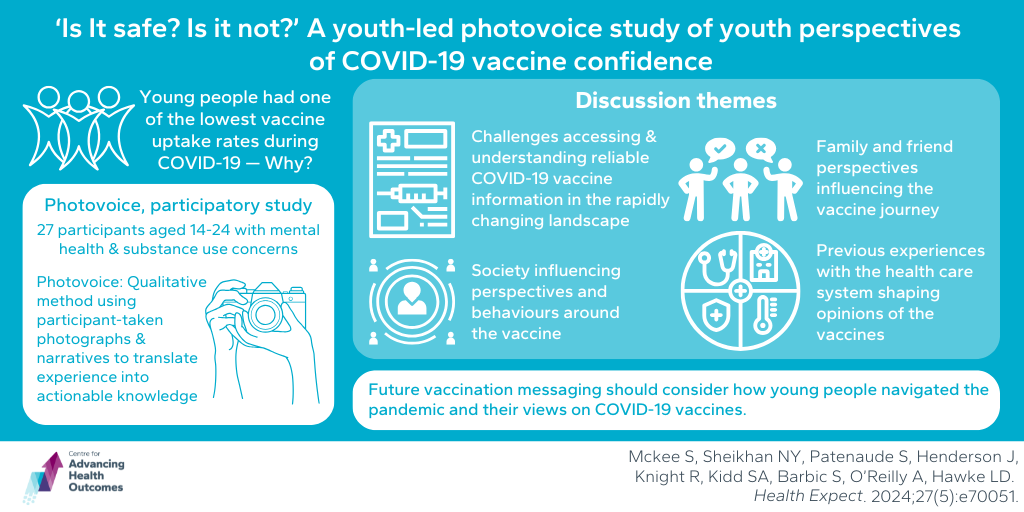
Youths’ perspectives of COVID-19 vaccines were influenced by a complex variety of external factors
Mckee S, Sheikhan NY, Patenaude S, Henderson J, Knight R, Kidd SA, Barbic S, O’Reilly A, Hawke LD. ‘Is it safe? Is it not?’ A youth-led photovoice study of youth perspectives of COVID-19 vaccine confidence. Health Expect. 2024;27(5):e70051.
During the COVID-19 pandemic, young people had one of the lowest rates of vaccine uptake, but why? Advancing Health Scientist Dr. Skye Barbic and colleagues conducted a photovoice, community-based participatory study to find out. They invited 27 young people aged 14–24 years with self-reported mental health and substance use concerns (MHSU) and current or past vaccine hesitancy to submit photographs and discuss their feelings about the pandemic and COVID-19 vaccines in focus groups. The researchers identified four key themes: 1) Challenges accessing and understanding reliable COVID-19 vaccine information in the rapidly changing landscape; 2) Family and friend perspectives influencing the vaccine journey; 3) Society influencing perspectives and behaviours around the vaccine; 4) Previous experiences with the health care system shaping opinions of the vaccines. Understanding how young people with MHSU navigated the pandemic and what impacted their perceptions of the COVID-19 vaccines should be considered when developing future public health messaging around vaccination.