Four new inflammatory airway disease trials are underway with the support of CHÉOS — staff will be providing coordinating and site management services. Dr. Del Dorscheid, a critical care and respiratory physician at St. Paul’s Hospital and researcher at the Centre for Heart Lung Innovation, is the principal investigator for all four of the studies.
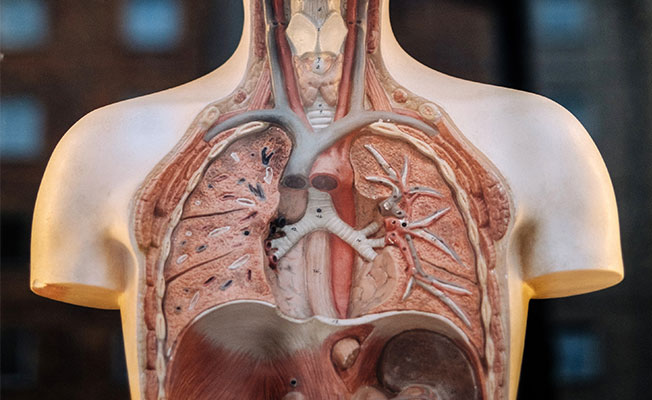
Three of the studies are examining treatment for asthma while the fourth is testing a novel treatment for chronic bronchitis, a form of chronic obstructive pulmonary disease (COPD). Lung disease affects millions of Canadians and significantly impacts the Canadian health care system; more than 3 million people in Canada are diagnosed with asthma and over 10 per cent of Canadians over the age of 40 have COPD. For many of these individuals, treating symptoms and managing disease remains difficult even when following treatment guidelines.

“When these chronic diseases aren’t well controlled, people end up needing more health care resources,” said Dr. Dorscheid. “This is costly to the health care system, but also creates indirect costs to society at large, and diminishes quality of life for those living with these conditions.”
Asthma treatments fall into one of two broad categories: long-term control medications, typically taken daily to reduce inflammation or keep airways open, and rescue medications that provide quick relief during an asthma attack. These asthma studies will be focusing on controller medications in individuals with severe asthma. Individuals with severe asthma, which make up about 5 to 10 per cent of all asthma cases, experience a greater frequency of exacerbations, decreased health-related quality of life, and worse symptoms. Newer therapies being developed for the treatment of severe asthma target specific molecules that generate the inflammation of the airway. These medications can improve health measures and reduce steroid exposure.
A Study of the Safety and Effectiveness of Benralizumab to Treat Patients with Severe Uncontrolled Asthma (ANDHI) is a study of the safety and effectiveness of the biologic therapy benralizumab, an anti-IL-5 treatment, in patients with eosinophilic asthma. St. Paul’s is one of over two hundred sites around the world where the phase III randomized, double-blinded, placebo-controlled study is taking place. Specifically, the study will measure the effect of benralizumab on the rate of asthma flare-ups, patient reported quality of life, and lung function as well as whether it can improve quality of life for those with chronic rhinosinusitis (sinus infection).
The second study is assessing a novel treatment for asthma, GSK3772847 an anti-IL-33 treatment. As a phase II study, the trial aims to evaluate the efficacy, safety, tolerability, pharmacokinetic, and pharmacodynamic profiles of GSK32772847. The study will be conducted in four phases: screening, run-in, treatment every four weeks, and follow-up. Both the intervention and placebo groups will also receive regular inhaler treatment twice daily as standard of care to assess the impact of this novel therapy.
Rather than assessing effectiveness as in the previous two studies, the Novartis Study will provide long-term safety data for the drug fevipiprant (QAW039) after being demonstrated as effective in reducing asthma attacks. It will compare the treatment at two different oral dosages to a placebo, when added to standard-of-care asthma therapy. Participants of previous trials will also be included in the study to provide data on extended exposure periods. This molecule is novel in that it heals the lining of the airway; Dr. Dorscheid is presently studying this drug in his lab using artificial airways.
Though these three studies are all testing therapies for asthma, each drug targets it via a different pharmacological mechanism. Asthma can be broken down into distinct subtypes based on the mechanisms driving disease. The variation in the causes of asthma requires unique approaches such as those tested in these studies.
“Because there are so many different factors underlying asthma, one drug isn’t going to work for everyone,” added Dr. Dorscheid. “Understanding what’s going on at a molecular or cellular level allows us to find ways to intervene in the different pathways that lead to disease in different people.”
Finally, the Gala Study is a feasibility trial that will be testing an innovative treatment for chronic bronchitis. The Gala airway treatment system is a device which uses high frequency short duration energy delivered using a catheter that runs through a bronchoscope to remove cells in the lining of the airway that overproduce mucus and make breathing difficult. The removal of abnormal airway lining cells then promotes the growth of healthy, normal tissue. The study will enroll and treat 24 participants from Vancouver and Montreal in order to assess the system’s safety and investigate a number of clinical outcomes. This study will be extended to include asthmatics in the fall of 2018.
“This study is exciting because there is no cure for chronic bronchitis and the treatment options are somewhat limited even for asthmatics that over produce airway mucous,” said Dr. Dorscheid. “Restoring the health of the airway tissue would be a major step forward in terms of treatment options that could improve quality of life for people with COPD and asthma.”
The ANDHI and Novartis studies have already started screening patients, while Gala and the GSK study will soon be underway.



