A new paper published by CHÉOS emergency medicine Scientists could reduce emergency department lengths-of-stay across the country.
Dr. Frank Scheuermeyer’s new publication in Academic Emergency Medicine focuses on the treatment of the most common heart rhythm disturbance, acute atrial fibrillation (AF), in the emergency department (ED), and compares the two treatment approaches currently used in Canada: an electrical-first strategy and a chemical-first strategy.
When a patient presents with AF, a physician will choose one of the two methods and, if it fails, will move on to the other method. Both treatment options have over 90% success rates, however, there has been considerable controversy in the medical community over which treatment regimen should constitute best practice. In Canada, a chemical-first approach is used in 56% of patients with the other 44% receiving electrical-first treatment.
“In Western Canada, we typically provide electrical stimulation followed by intravenous medication, if needed; in Eastern Canada, the treatments are provided in the opposite order” noted Dr. Jim Christenson, CHÉOS Scientist and study co-author.

To provide some empirical insight to the controversy, the research team conducted a six-centre randomized trial with included St. Paul’s and Mount St. Joseph’s Hospitals. The team hypothesized that an electrical-first strategy would be faster and as safe as a chemical-first method.
The group randomized 84 consenting patients with uncomplicated AF to receive treatment starting with either a procainamide infusion or electrical cardioversion strategy. The primary outcome for the trial was the proportion of patients in each arm that were discharged within four hours of ED arrival. To limit treatment bias, attending physicians in all the participating EDs were not made aware of the study’s outcome of focus.
Furthermore, the writing of the manuscript for the publication of the study results was blinded. This means that the researchers received the data for each arm without knowing which was arm was electrical-first or chemical-first. Two manuscripts were written and only after they were approved by all authors was the blinding of the treatment removed. This approach helps to ensure that the final submission was written in a fair and measured way and to avoid any editorializing about the two treatments.
“We found that both methods were equally safe but that providing electrical stimulation first, rather than the chemical method, results in earlier patient discharges” said Dr. Frank Scheuermeyer, the study’s lead author.
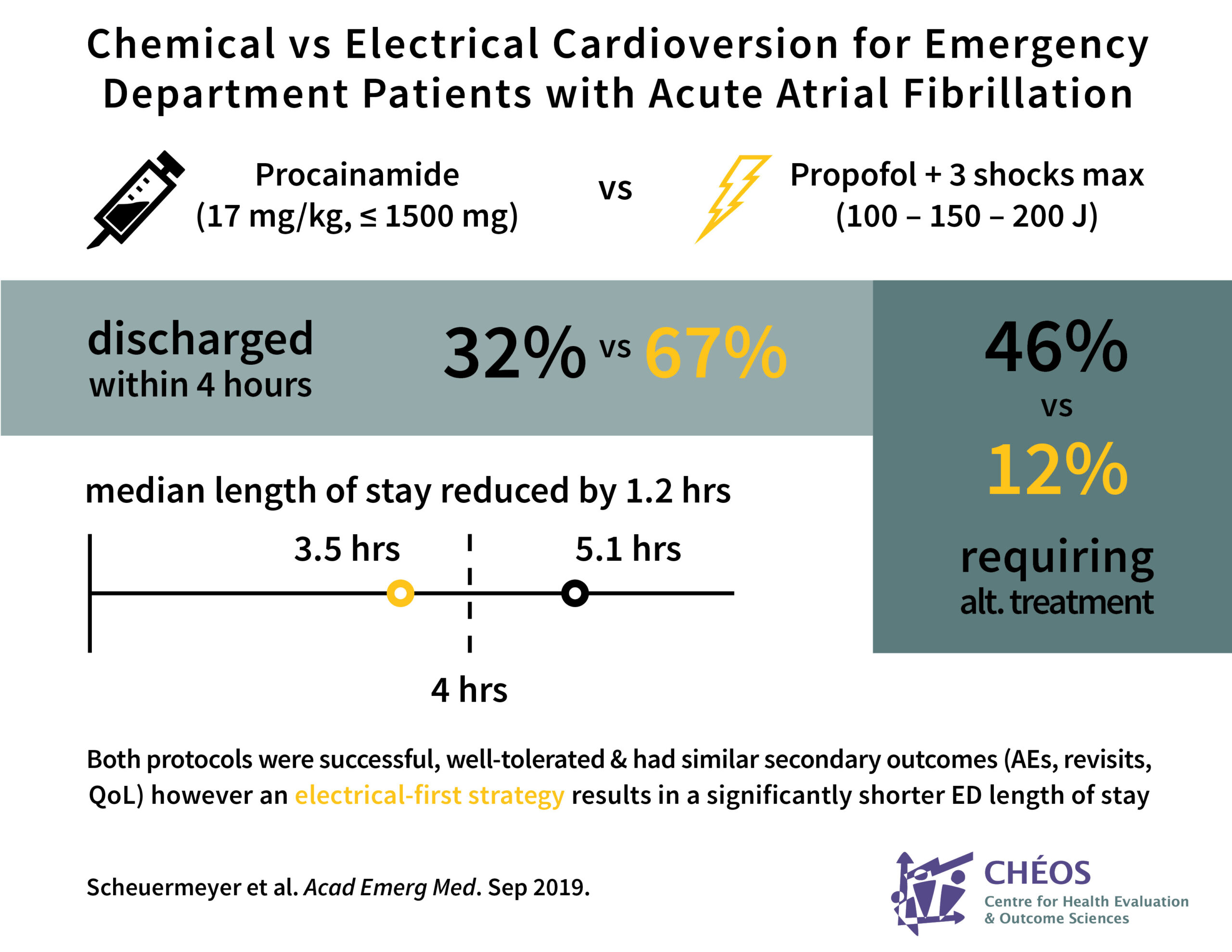
Specifically, the group found that 13 of 41 patients (32%) in the chemical group were discharged within 4 hours compared to 29 of 43 (67%) in the electrical group. The median length of stay in the emergency department was 5.1 hours in the chemical group compared to 3.5 hours in the electrical group, a median difference of 1.2 hours. All other outcomes were similar, including adverse events, return visits to the ED, and quality of life at 3 and 30 days after treatment.
Strategies needed to reduce wait times
As an area of hospital medicine that can be considerably strained by wait times and overcrowding, systems that lead to safe, earlier discharges can be very beneficial and cost saving. According to a report released by the Canadian Institute of Health Information, ED length of stay for people admitted in 2016-17 was up 11% from the year before and almost 17% from 5 years prior.
“An hour’s decrease in length of stay for a common arrhythmia could have a significant impact on wait times,” noted Dr. Scheuermeyer, “Our study provides strong evidence and rationale for standardizing the way emergency departments handle atrial fibrillations across Canada.”
A number of strategies to reduce wait times in the ED have been proposed and tested, including a strategy to change physician payment structures published last year by Dr. Scheuermeyer and two other CHÉOS Scientists, Drs. Rob Stenstrom and Eric Grafstein. Upcoming studies will focus on recent changes in the evaluation of chest pain patients at St. Paul’s and Mount St. Joseph’s Hospitals.
Dr. Scheuermeyer is the Interim Director of Research at the St. Paul’s Hospital Emergency Department and the Program Head for Emergency Medicine at CHÉOS. More information about the study can be found on clinicaltrials.gov.
The publication was chosen as the editor’s pick for the September edition of the journal. Visit EurekAlert! to find a press release about this study.



