The Evidence Speaks Series is a recurring feature highlighting the latest in CHÉOS research. This series features summaries of select publications as well as in-depth features on the latest work from our investigators. In the early days of CHÉOS, the Centre had a series known as “The Evidence Speaks,” a monograph series to keep media and the research community up-to-date with CHÉOS’ current research results in the health outcomes field.
Maas ET, Koehoorn M, McLeod CB. Return-to-work for multiple jobholders with a work-related musculoskeletal disorder: A population-based, matched cohort in British Columbia.PLoS ONE. 2018 Apr 3;13(4):e0193618.
As many as 132,000 workers in B.C. (5.5% of the workforce) may hold multiple jobs, a practice which can increase risk of injury due to factors such as fatigue, longer hours, and less leisure time. Although multiple job holders are less likely to be absent from work due to illness, little is known about the impact of working multiple jobs on return to work after injury. In this study, CHÉOS Scientist Dr. Mieke Koehoorn, with researchers from the Partnership for Work at UBC, compared the impact of musculoskeletal disorders (MSDs) between people with single and multiple jobs. In Canada, MSDs account for the highest disability costs due to productivity loss and the burden of disease from MSDs is expected to increase with an aging Canadian population. Administrative data from WorkSafeBC and B.C.’s provincial workers’ compensation system were used for this study. Between January 2010 and December 2014, claims data were used to identify 140,371 single jobholders and 10,168 multiple jobholders with MSD injuries. A matched sample totaling 16,678 individuals (8,389 each for single and multiple jobholders) was also identified. On average, 6.71% of multiple job holders had a claim due to a work-related MSD, notably higher than the portion of the workforce they represent (5.5%). Multiple jobholders were also more likely to be women, have a higher income, work in a health and services occupation, and to experience fractures. Analysis of the matched sample showed that multiple jobholders were less likely to return to work within the first six months after an MSD claim. The impact of holding multiple jobs on return to work was more pronounced in men; this result may be due to the tendency for men to supplement a full-time job with a second part-time job while women are more likely to have two part-time jobs. In general, workers who worked six or seven days per week prior to their injury were less likely to return to work. The authors suggest that the differences in return to work in single versus multiple jobholders is due to a higher workload, a decreased likelihood of multiple jobholders to submit a workers’ compensation claim, and less access to modified work upon return. This research highlights the need for interventions and support for those at risk of a delayed return to work following MSD injury.
—
Khan NA, Rabkin SW, Zhao Y, McAlister FA, Park JE, Guan M, Chan S, Humphries KH. Effect of lowering diastolic pressure in patients with and without cardiovascular disease. Hypertension. 2018 Mar 26 epub ahead of print.
The Systolic Blood Pressure Intervention Trial (SPRINT) showed that, in those with high risk of cardiovascular disease, systolic blood pressure (SBP) below 120 mmHg (compared to a standard target of <140 mmHg) was associated with reduced cardiovascular (CV) events and mortality. However, healthcare providers were reluctant to lower the BP threshold due to the risk of adverse events if BP falls too low. This led Drs. Nadia Khan and Karin Humphries, with other researchers from UBC, to analyze the data from the SPRINT trial to identify the relationship between lower SBP and diastolic blood pressure (DBP) on CV events, and to identify predictors of developing low BP. In the trial, patients were randomized to either intensive BP lowering (<120 mmHg) or standard lowering (<140 mmHg).
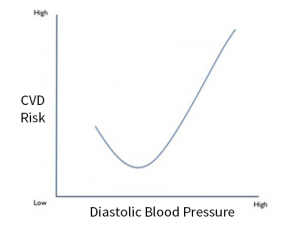
Seven thousand five hundred and seventy-four (7574) patients without cardiovascular disease (CVD) and 1519 patients with CVD were included in the secondary analysis. The researchers found that diastolic blood pressure below 55 mmHg or above 95 mmHg was associated with an increased risk of CV events, in what is known as a J-shaped relationship. No such relationship was found for SBP. Factors that predict a treatment response of DBP below 55 mmHG included being male, being older, a history of CVD, and lower baseline DBP. This research suggests that clinicians and patients should be cautious when trying to achieve intensive
blood pressure targets, particularly in those
with the identified predictive factors.
—
Snow ME, Tweedie K, Pederson A. Heard and valued: The development of a model to meaningfully engage marginalized populations in health services planning. BMC Health Serv Res. 2018 Mar 15;18(1):181.
Including patient voices in the decision-making process for health services and policy development is essential. The benefits of patient engagement is lost if patients are not included in a meaningful way or the process does not properly incorporate their values, preferences, and needs. CHÉOS’ Dr. Beth Snow, with researchers from UBC and BC Women’s Hospital, recently published a qualitative analysis and planning model to improve engagement of marginalized women, a group whose engagement in research has not been appropriately facilitated in the past. The group conducted a literature review as well as focus groups and interviews with community members, health service planners, and researchers who had previous experience in patient engagement. The model that was developed out of the qualitative work highlights the need for health care planners to consider how gender in combination with other factors may limit participation. Both planners and patients expressed the importance of developing engagement methods that match the abilities and preferences of those participating, rather than those of health planners. Identified barriers to participation included costs of participation (parking, child care) and opportunity cost relating to loss of work or social opportunities. The researchers concluded that engagement processes must be adapted to particular situations and sets of barriers. To assist health systems planners in the use of this model, both printed and online training materials were developed.



