The Evidence Speaks Series is a recurring feature highlighting the latest in CHÉOS research. This series features summaries of select publications and is designed to keep media and the research community up to date with CHÉOS’ current research results in the health outcomes field.
To ensure this research is quick and easy to share, we are now providing social cards that you are free to save and use as you see fit.
Fostering compassion in clinical environments could support the delivery of collaborative care in eating disorders treatment
Geller J, Fernandes A, Kelly AC, Samson L, Srikameswaran S. Collaborative care in eating disorders treatment: exploring the role of clinician distress, self-compassion, and compassion for others. J Eat Disord. Published online April 6, 2023.
Collaborative care, which focuses on supporting patient choice and autonomy, is an important aspect of evidence-based clinical practice and contributes to better treatment outcomes than directive care, when clinicians’ opinions direct the care pathway without input from the patient. A collaborative approach is particularly important in the treatment of eating disorders where it is linked to higher motivation for change. However, despite evidence supporting a collaborative approach, clinicians and care teams sometimes use a directive approach instead, where patients have limited influence over their treatment plan resulting in negative attitudes toward treatment and lower levels of adherence. In this study, Dr. Josie Geller and colleagues examined the impact of how clinicians experience and manage distress on their delivery of collaborative support. The results showed that clinicians’ self-compassion and compassion for others were associated with greater use of collaborative support. Clinicians’ personal experience of distress was not related to the manner in which they offered support. These findings suggest that fostering compassion through educational interventions may be beneficial for health care providers to improve their ability to deliver collaborative care.

—
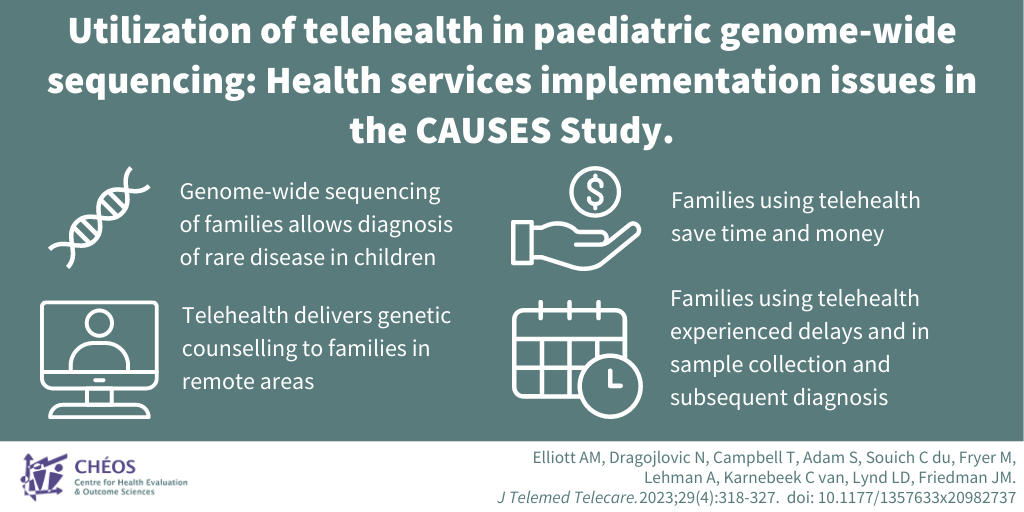
Telehealth allows for access to genome-wide sequencing for families in remote communities
Elliott AM, Dragojlovic N, Campbell T, Adam S, Souich C du, Fryer M, Lehman A, Karnebeek C van, Lynd LD, Friedman JM. Utilization of telehealth in paediatric genome-wide sequencing: Health services implementation issues in the CAUSES Study. J Telemed Telecare. 2023 May;29(4):318-327.
Genome-wide sequencing (GWS) is transforming the care and management of paediatric patients with a rare disease because of its diagnostic capabilities. GWS is particularly effective when both parents and the child are sequenced as a trio. Pre-test genetic counselling is recommended for families considering GWS. This demand imposes increasing pressure on an already strained resource. Alternative methods, including telehealth, are necessary to meet clinical demands, particularly for families living in remote communities. CHÉOS’ Dr. Larry D. Lynd and team compared health services experiences and issues between families seen onsite versus remotely for pre-test genetic counselling. They found that while telehealth allowed access to genome-wide sequencing for families in remote communities and saved significant travel and time costs, there was a significant delay in sample collection in the telehealth group. This delay impacted the time to result reporting, and to diagnosis for families for whom GWS was diagnostic. This delay needs to be considered particularly in families where rapid diagnosis is essential for immediate changes in medical management. However, in many of these urgent cases, families are often already at the care centre so a delay in sample collection is less likely.
—
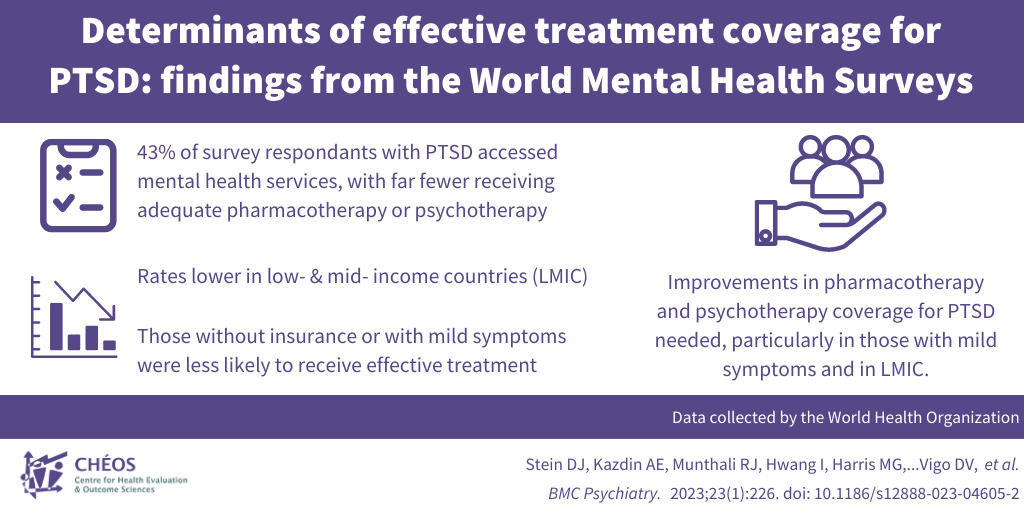
Pharmacotherapy and psychotherapy coverage for PTSD could be improved, particularly for those with mild symptoms and in low- and middle-income countries
Stein DJ, Kazdin AE, Munthali RJ, Hwang I, Harris MG,…Vigo DV, et al. Determinants of effective treatment coverage for posttraumatic stress disorder: findings from the World Mental Health Surveys. BMC Psychiatry. 2023 Apr 4;23(1):226.
Post-traumatic stress disorder (PTSD) is a psychiatric disorder that may develop because of exposure to a traumatic event. PTSD is associated with significant morbidity, individual suffering, reduced quality of life, and considerable societal costs. Fortunately, a variety of effective pharmacotherapy and psychotherapy treatments are available. In this study involving CHÉOS Scientist Dr. Daniel Vigo, data from the World Mental Health Surveys, conducted by the World Health Organization (WHO), was used to investigate how many patients with PTSD received adequate treatment (pharmacotherapy and/or psychotherapy) according to the severity of their condition. The study found that 43 per cent of people with PTSD received any mental health services, with far fewer receiving adequate pharmacotherapy or psychotherapy (13.5 and 17.2 per cent, respectively). These rates were lower in low- and middle-income countries (LMIC) than in high-income countries (HIC). Those without insurance or with mild clinical symptoms were less likely to receive effective treatment coverage for PTSD. This study indicates a need to improve pharmacotherapy and psychotherapy coverage for PTSD, particularly in those with mild symptoms and in LMIC and suggests that universal health care insurance for both physical and mental disorders are key to addressing barriers to effective care.