The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
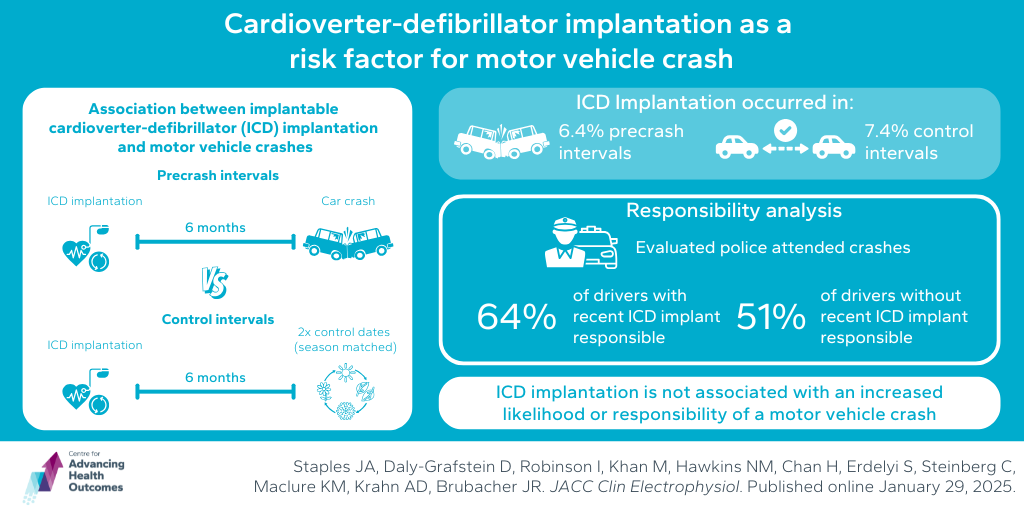
Recent implantable cardioverter-defibrillator implantation is not associated with an increased risk of motor vehicle crash
Staples JA, Daly-Grafstein D, Robinson I, Khan M, Hawkins NM, Chan H, Erdelyi S, Steinberg C, Maclure KM, Krahn AD, Brubacher JR. Cardioverter-Defibrillator Implantation as a Risk Factor for Motor Vehicle Crash. JACC Clin Electrophysiol. Published online January 17, 2025.
Due to the risk of complications in the first few months after implantable cardioverter-defibrillator (ICD) implantation, many jurisdictions require patients to temporarily cease driving after the operation. However, these policies are based on limited and methodologically flawed studies. To inform policies about driving restrictions after ICD implantation, Advancing Health Scientist Dr. John Staples led a study to determine if there is an association between ICD implantation and motor vehicle crashes. The researchers looked at all the people in BC with an ICD implantation involved in a crash over a 12-year period. They compared the likelihood that ICD implantation occurred within a 6-month period prior to the crash (precrash intervals) to the likelihood that implantation occurred within a 6-month period of two seasonally matched control dates (control intervals). In this study design, if crashes are preceded by ICD implantation more often than would be expected by chance, it could identify ICD implantation as a risk factor for crash. Analyses revealed that ICD implantation occurred in 6.4 per cent of precrash intervals and 7.4 per cent of control intervals. Further analysis looked at every driver involved in a police-attended crash between 1997 and 2019 to determine driver responsibility. This showed that 64 per cent of drivers with recent ICD implantation and 51 per cent of drivers without recent ICD implantation were determined to be responsible for their crash. The researchers concluded that ICD implantation is not associated with an increased likelihood of motor vehicle crash in the subsequent six months and does not increase the likelihood of crash responsibility.
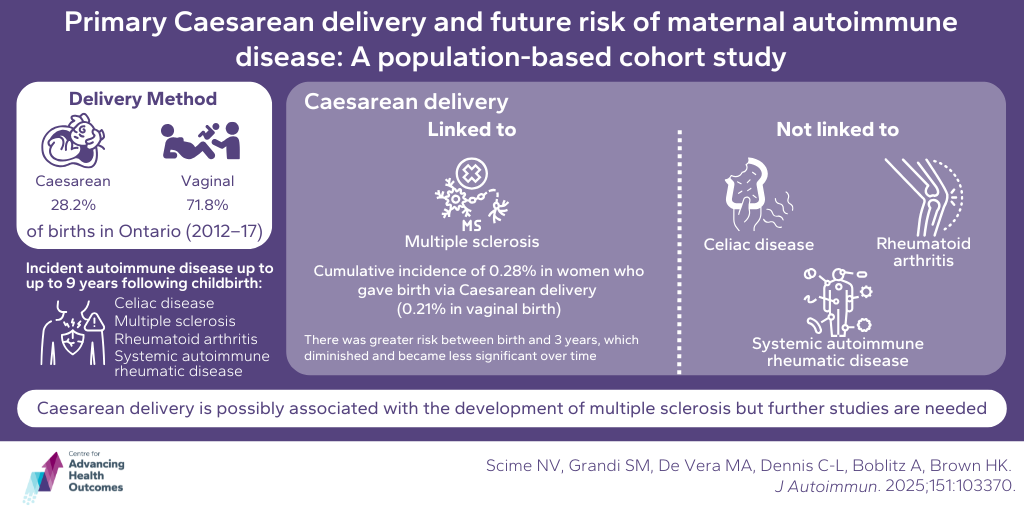
Multiple sclerosis may be more likely in women who give birth via a Caesarean
Scime NV, Grandi SM, De Vera MA, Dennis C-L, Boblitz A, Brown HK. Primary Cesarean delivery and future risk of maternal autoimmune disease: A population-based cohort study. J Autoimmun. 2025;151:103370.
Caesarean section has been hypothesized to increase a women’s risk of autoimmune disease later in life, but existing evidence is unclear. A team of researchers from BC and Ontario, including Advancing Health’s Dr. Mary De Vera, recently published research on this possible association. Of 253,901 women in Ontario who gave birth to their first child between 2012 and 2017, 28.2 per cent gave birth through Caesarean delivery, while 71.8 per cent gave birth vaginally. At up to 9 years following childbirth, the data indicated that Caesarean delivery was associated with an increased risk of multiple sclerosis (MS; occurring in 0.28 per cent of women who gave birth via Caesarean delivery), but not rheumatoid arthritis (RA), systemic autoimmune rheumatic disease (SARD), or coeliac disease. In comparison, 0.21 per cent of women who gave birth vaginally developed MS. Furthermore, the association with MS was strongest in the first three years after birth. The researchers concluded that, while Caesarean delivery is possibly linked with the development of MS, further studies are warranted.
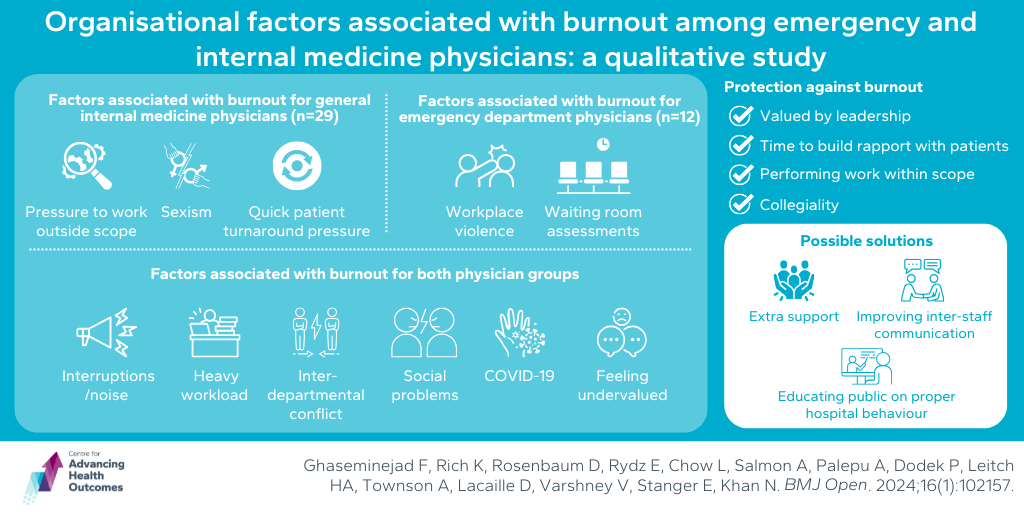
Physicians lend their perspectives on how burnout could be reduced in BC hospitals
Ghaseminejad F, Rich K, Rosenbaum D, Rydz E, Chow L, Salmon A, Palepu A, Dodek P, Leitch HA, Townson A, Lacaille D, Varshney V, Stanger E, Khan N. Organisational factors associated with burnout among emergency and internal medicine physicians: a qualitative study. BMJ Open. 2025;15(1):e085973.
Previous research has shown that at least two-thirds of emergency department (ED) and general internal medicine (GIM) physicians experience burnout. In this recent study, Advancing Health’s Drs. Amy Salmon, Anita Palepu, Peter Dodek, Nadia Khan, and colleagues, set out to gather physicians’ perspectives on system-specific issues that contribute to burnout, factors that are protective, and possible solutions. Speaking with 29 GIM and 12 ED physicians in Vancouver, BC, the research team determined that factors associated with burnout among both groups included interruptions and noise, interdepartmental conflict, heavy workload, feeling undervalued, social problems, and COVID-19. GIM physicians also disclosed that pressure to work outside of their scope of practice, pressure for quick patient turnaround, and sexism also contributed to burnout, while ED physicians said that workplace violence and having to assess patients in waiting rooms were also factors. Major themes identified that protected against burnout were feeling valued by leadership, having time to build a rapport with patients, collegiality, and performing work within their scope of practice. Possible solutions to relieve burnout include extra support to relieve heavy workload and scheduling, hiring more staff to assist with non-physician roles, educating the public on appropriate behaviour in the hospital, and improving inter-staff communication. In all, this paper highlighted a significant amount of crossover between factors that lead to burnout among GIM and ED physicians. Furthermore, there are numerous possible steps the health care system could take to improve and protect physicians going forward.