The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
Virtual care may help remove barriers to effective HIV care
Mbuagbaw L, Fernando S, Lee C, Owino M, Youssef C, Snow ME. Barriers and facilitators to improving the cascade of HIV care in Ontario: a mixed method study. BMC Health Services Research. Published online January 10, 2024.
Advancing Health Program Head of Evaluation, Dr. Beth Snow, and Qualitative Methodologist, Saranee Fernando, worked with colleagues to identify barriers and facilitators to implementing effective HIV care cascade strategies in Ontario, Canada. The team had previously identified effective care strategies that improve initiation of antiretroviral therapy (ART), adherence to ART, and retention in care, including mobile health interventions, incentives, education, and counselling. This study used a mixed methods approach, including a survey and in-depth interviews with health workers and people living with HIV (PLWH). The results showed that Ontario clinics implemented various evidence-based interventions to improve engagement in care, despite concerns about resources. Barriers such as physical and financial access to care, workload for tailored care, and lack of expertise were identified, while facilitators included virtual care and client preparedness through education and peer support. The study highlighted the need for more health workers with skills to address the unique needs of PLWH and the benefits of virtual care for both health workers and PLWH. This research provides valuable insights into the challenges and opportunities in enhancing HIV care in Ontario and contributes to the broader conversation on patient engagement and the HIV care cascade, shedding light on the complexities and potential solutions in this critical area of health care.

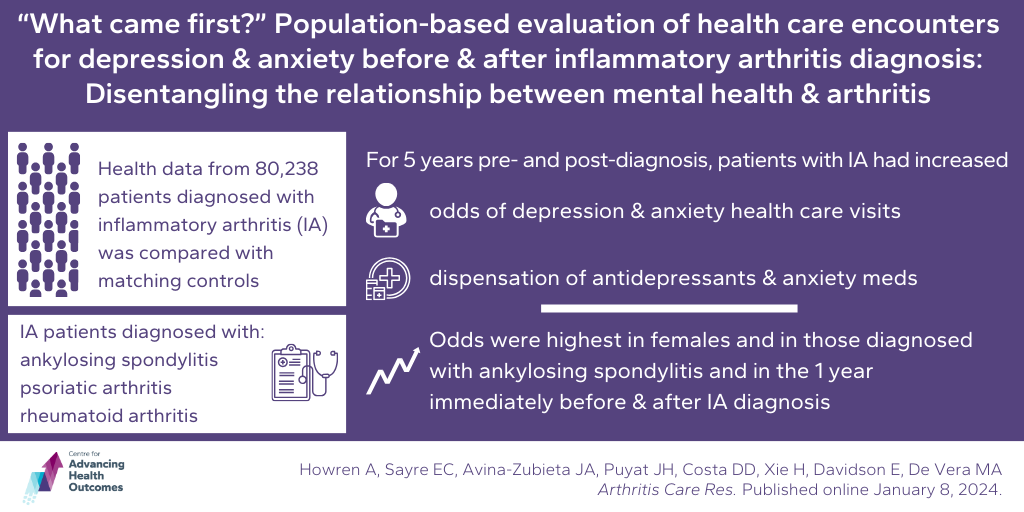
Depression and anxiety may characterize the early stages of inflammatory arthritis
Howren A, Sayre EC, Avina-Zubieta JA, Puyat JH, Costa DD, Xie H, Davidson E, De Vera MA. “What came first?” Population-based evaluation of health care encounters for depression and anxiety before and after inflammatory arthritis diagnosis: Disentangling the relationship between mental health and arthritis. Arthritis Care Res. Published online January 8, 2024.
This study aimed to understand the patterns of depression and anxiety health care use before and after the diagnosis of inflammatory arthritis (IA) in patients with ankylosing spondylitis, psoriatic arthritis, and rheumatoid arthritis. Drs. Joseph Puyat and Mary De Vera, from Advancing Health, along with colleagues, analyzed health data from 80,238 people with IA in B.C. and a matching number of people without IA. They found that patients with IA had significantly higher odds of health care visits related to depression and anxiety and were more likely to be prescribed antidepressants and anti-anxiety medications both five years before and five years after IA diagnosis. These outcomes were more likely in the year immediately before or after the IA diagnosis. Encounters were more pronounced in those diagnosed with ankylosing spondylitis compared to other types of IA, and amongst females compared to males. The results suggest that there is a connection between depression, anxiety, and IA, indicating a potential role for these mental health conditions in the development of IA. The findings also propose hypotheses about the interrelated biological, psychological, and social processes linking IA and mental health comorbidities. The study provides valuable insights into the relationship between mental health and inflammatory arthritis, highlighting the importance of addressing mental health in the context of IA diagnosis and treatment.
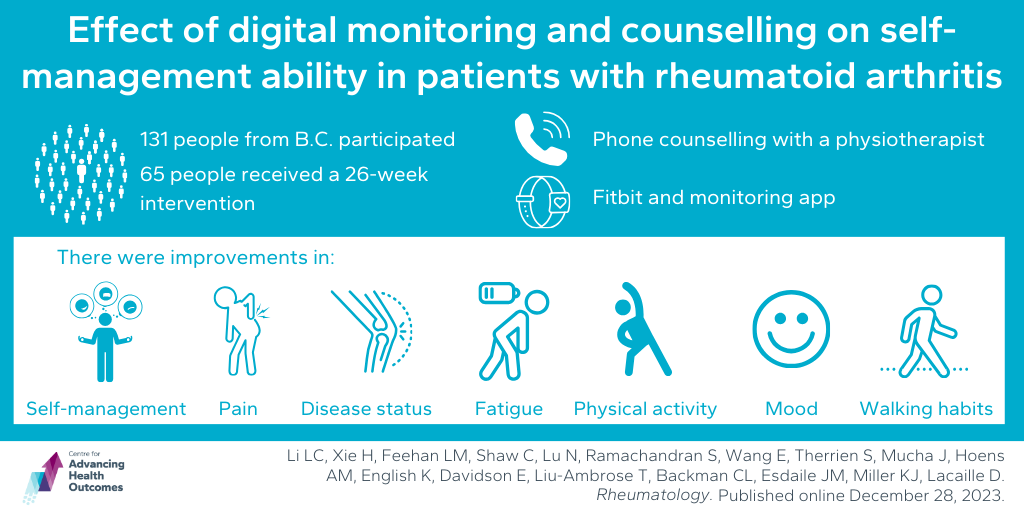
Remote physiotherapist counselling combined with self-monitoring tools may improve rheumatoid arthritis symptom management
Li LC, Xie H, Feehan LM, Shaw C, Lu N, Ramachandran S, Wang E, Therrien S, Mucha J, Hoens AM, English K, Davidson E, Liu-Ambrose T, Backman CL, Esdaile JM, Miller KJ, Lacaille D. Effect of digital monitoring and counselling on self-management ability in patients with rheumatoid arthritis: a randomised controlled trial. Rheumatology (Oxford). Published online December 28, 2023.
This study, by Advancing Health Scientist Dr. Linda Li and Research Associate Alison Hoens, and colleagues, aimed to evaluate the effectiveness of a remote physiotherapist (PT) counselling intervention, along with self-monitoring tools, in improving self-management, physical activity, and health outcomes in people with rheumatoid arthritis (RA). The participants were randomly assigned to receive immediate intervention, including group education, a Fitbit, a self-monitoring app, and PT counseling phone calls, or a delayed intervention (intervention introduced at 17 weeks). The team looked at the impact of the intervention on ability to self-manage their RA, disease status, pain, fatigue, physical activity, and mood. The results showed that the immediate intervention group demonstrated a significant improvement in the ability to self-manage over 27 weeks compared to the delayed group. Additionally, the intervention also had favourable effects on disease activity, fatigue, depression, and self-reported walking habits. These results suggest that remote counselling combined with self-monitoring tools improved self-management ability in individuals with RA and had a positive effect on symptom management.