The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
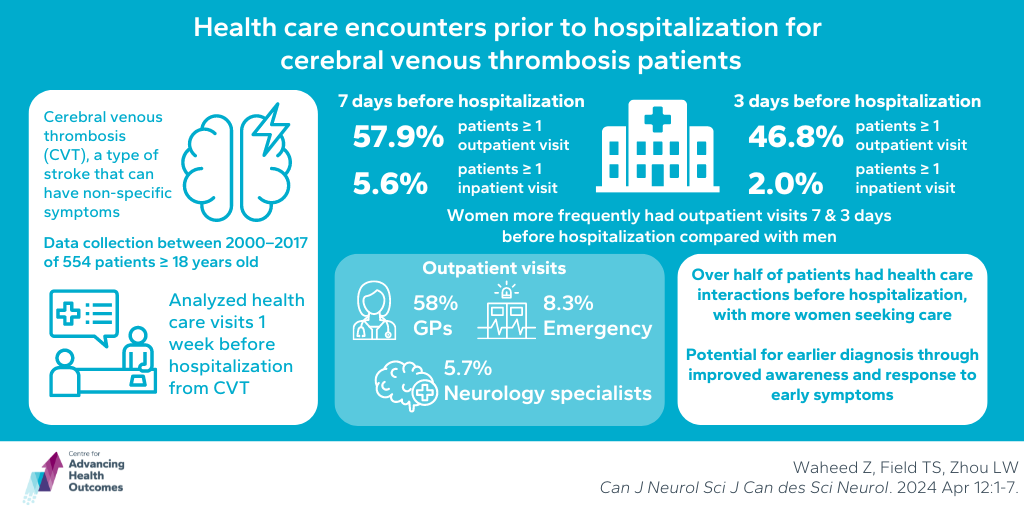
Exercise and social communication promote mental wellness by reducing anxiety symptoms
Cheong Q, Kazanjian A, Puyat JH. Easing anxiety symptoms through leisure activities during social isolation: Findings from nationally representative samples. PLOS ONE. 2024;19(6):e0303585. doi:10.1371/journal.pone.0303585
Public health measures during the COVID-19 pandemic led to exacerbated anxiety symptoms for many. Advancing Health Scientist Dr. Joseph Puyat led a study exploring how leisure activities can support mental wellness during social isolation and times of limited access to recreational and mental health services. The research examined survey data from Statistics Canada, collected in early May and late July 2020, to determine the relationship between leisure activities and anxiety symptoms. This was done by evaluating participants who did or did not engage with leisure activities (communication with friends and family, meditation, exercise) in those who self-reported experiencing moderate to severe anxiety on the Generalized Anxiety Disorder 7-item anxiety scale. The most common leisure activities reported were exercise and communicating with friends and family. Anxiety symptoms were less common in July than in May. Regression analysis showed that exercise and communication with family were linked to lower prevalence of anxiety symptoms, while meditation was linked to a higher prevalence of anxiety symptoms in both May and July, which might be due to repetitive negative thinking as a result of traumatic stress from the pandemic. The study concludes that exercise and social communication can help promote mental wellness by reducing anxiety symptoms, and further research should investigate the impact of meditation on mental health during social isolation.
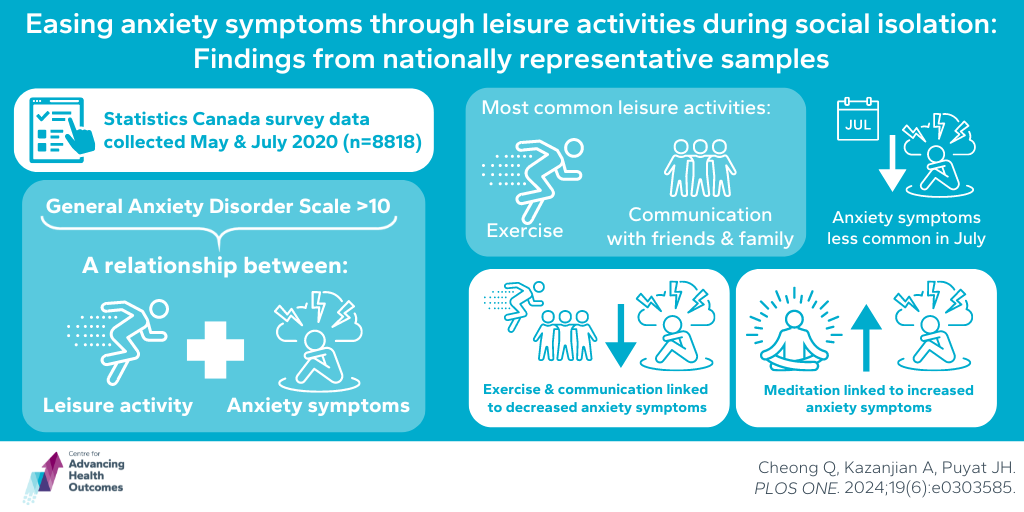
Foraging walks promote heart health within Squamish Nation
Oppliger K, Blair S, Price R, Nahanee M (Latash), Nahanee D, Duncan R (Tsitsáyx̱emaat), Lamont E, Beverly A, Dawson A (Spelexilh), Conklin AI. Promoting Slhánay̓ Sḵwálwen (Indigenous Women’s Heart Health): Findings from sharing circles with Squamish Nation. J Nutr Educ Behav. Published online 2024. doi:10.1016/j.jneb.2024.04.003
There is limited knowledge evaluating culturally safe and environmental approaches to nutrition education and cardiovascular health awareness in Indigenous communities. Advancing Health Scientist Dr. Annalijn Conklin, with input and leadership from members of the Squamish Nation, aimed to develop a model to improve the understanding of heart health and increasing heart health awareness by integrating this knowledge with land-based practices. These community-led foraging walks serve as a culturally safe way to educate participants about nutrition, as they reported previous mistreatment and judgement by health professionals. Participants, who mostly had limited foraging experience, expressed a strong desire to learn about traditional foods and noted a lack of heart health-related nutrition education. They highlighted key elements for future programs, including involvement, implementation, and ideal settings. All agreed that foraging walks help promote five dimensions of heart health — physical, emotional, spiritual, mental, and social — through physical activity, purposeful nutrition, and connection to community and culture. The findings informed a template for future sessions and plant identification cards for the community. This study suggests the need for pilot programs and further research on heart health and land-based practices tailored to different Indigenous groups nationally.
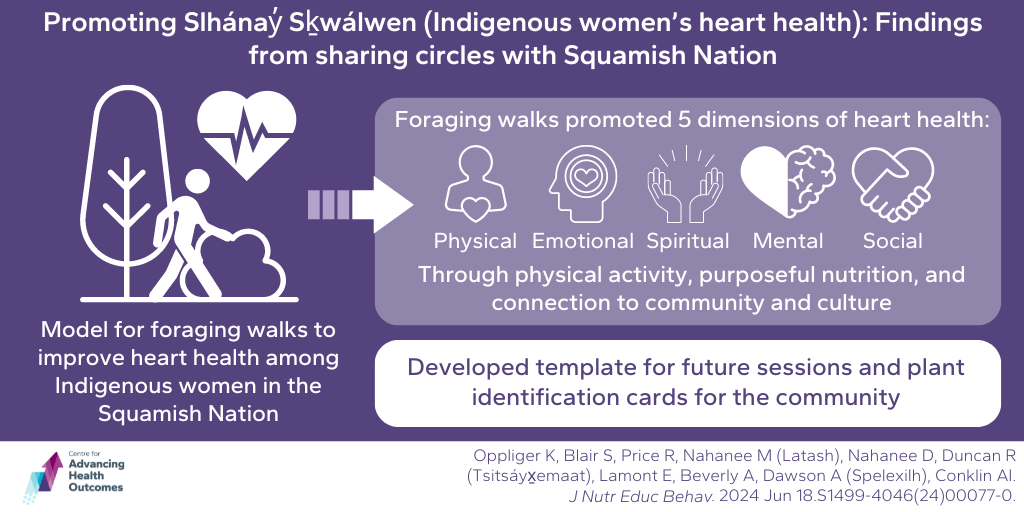
Potential for early diagnosis of cerebral venous thrombosis during outpatient visits
Waheed Z, Field TS, Zhou LW. Health care encounters prior to hospitalization for cerebral venous thrombosis patients. Can J Neurol Sci J Can des Sci Neurol. Published online June 13, 2024:1-7. doi:10.1017/cjn.2024.48
Unlike other causes of stroke, cerebral venous thrombosis (CVT) symptoms can be nonspecific at onset and then gradually worsen over time. To explore potential opportunities for earlier diagnosis, Advancing Health Scientist Dr. Lily Zhou examined the health care interactions of patients in BC prior to their hospitalization with CVT. Using linked patient-level administrative and registry data from 2000 to 2017, health care visits of 554 patients throughout BC aged 18 and older were analyzed in the week before hospitalization for CVT. Findings revealed that 57.9 per cent of patients had at least one outpatient visit and 5.6 per cent had at least one inpatient visit within seven days before hospitalization. In the three days before hospitalization, 46.8 per cent had outpatient visits and 2.0 per cent had inpatient visits. Women were more likely than men to have outpatient visits in the seven days and three days before hospitalization. Most outpatient visits were with general practitioners (58.0 per cent), followed by emergency (8.3 per cent) and neurology (5.7 per cent) specialists. The study concluded that over half of the patients had health care interactions in the week before their CVT hospitalization, with women being more likely to seek outpatient care. It is uncertain if the differences in health care use are due to health-seeking behaviour, intrinsic CVT symptoms, or physicians’ interpretation of symptoms. However, this suggests a potential for earlier diagnosis through improved awareness of early symptoms and redirection of at-risk patients for urgent diagnostic imaging.