The Evidence Speaks Series is a recurring feature highlighting the latest in CHÉOS research. This series features summaries of select publications and is designed to keep media and the research community up to date with CHÉOS’ current research results in the health outcomes field.
To ensure this research is quick and easy to share, we are now providing social cards that you are free to save and use as you see fit.
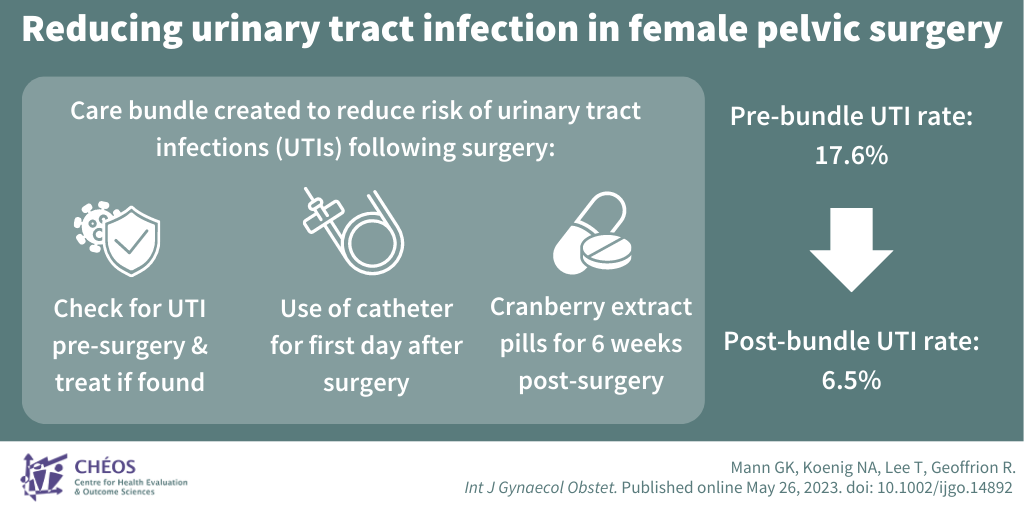
A clinical bundle can decrease UTI rates and hospital stay threefold after pelvic reconstructive surgery
Mann GK, Koenig NA, Lee T, Geoffrion R. Reducing urinary tract infection in female pelvic surgery: A retrospective cohort study. Int J Gynaecol Obstet. Published online May 26, 2023.
Incidence of urinary tract infections (UTIs) following female pelvic reconstructive surgery ranges from 7 to 34 per cent. Reducing UTIs in women following surgery is important for patient health and well-being, and for reducing health care costs. In this study, a team including CHÉOS’ Dr. Roxana Geoffrion explored the implementation and effectiveness of a care bundle aimed at reducing UTIs in this group of patients. The care bundle included consisted of three interventions designed to reduce the risk of infection: Checking for UTIs before surgery and treating them if found; using a catheter after surgery instead of trying to urinate right away; and taking cranberry extract pills for six weeks after surgery. The researchers compared the rates of UTIs in patients before and after the care bundle was implemented and found that the care bundle significantly reduced the rate of postoperative UTIs from 17.6 per cent in the pre–bundle group to 6.5 per cent in the post–bundle group. This intervention improves patient outcomes and decreases the length of hospital stay for patients and may reduce health care costs.
 —
—
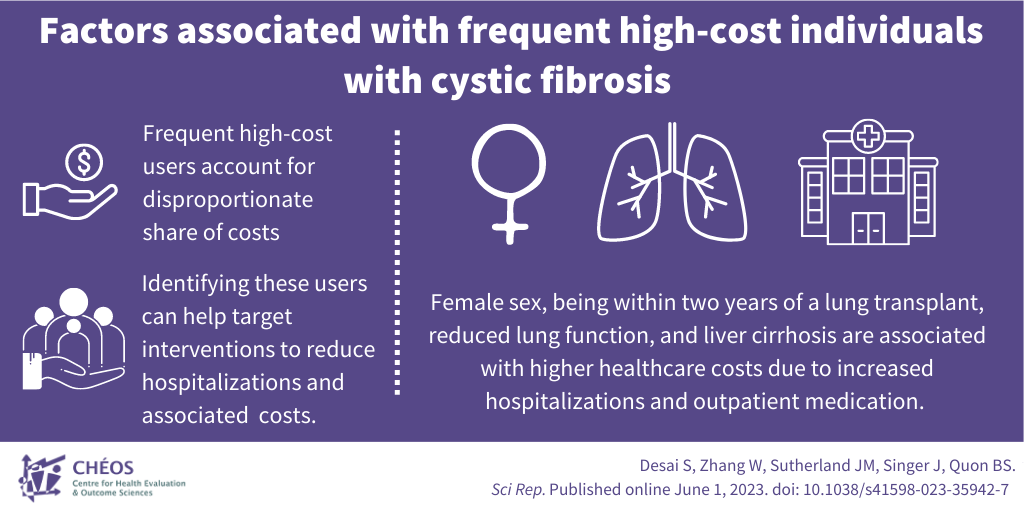
Interventions targeting frequent high-cost CF users may reduce health care costs
Desai S, Zhang W, Sutherland JM, Singer J, Quon BS. Factors associated with frequent high-cost individuals with cystic fibrosis and their healthcare utilization and cost patterns. Sci Rep. Published online June 1, 2023.
In this paper, CHÉOS’ Sameer Desai, and Drs. Wei Zhang, Jason Sutherland, and Joel Singer explored the health care costs and use associated with cystic fibrosis (CF) care in B.C. Using data from the Canadian Cystic Fibrosis Registry and multiple administrative databases, they analyzed the costs over time to identify factors associated with frequent high-cost CF users. Health care costs for CF care have been increasing over the years, primarily driven by expensive specialty drugs and nebulized therapies. The study identifies demographic and clinical factors, such as age, sex, lung function, and complications, that are associated with becoming a frequent high-cost CF user. Female sex, being within two years of a lung transplant, reduced lung function, and liver cirrhosis are found to be factors associated with higher health care costs due to increased hospitalizations and the need for more intensive treatment. Understanding the drivers of health care costs and recognizing segments of the CF population who use a disproportionate amount of health care resources can help to target interventions, for example earlier liver transplants, may reduce hospitalizations and associated health care costs.
—
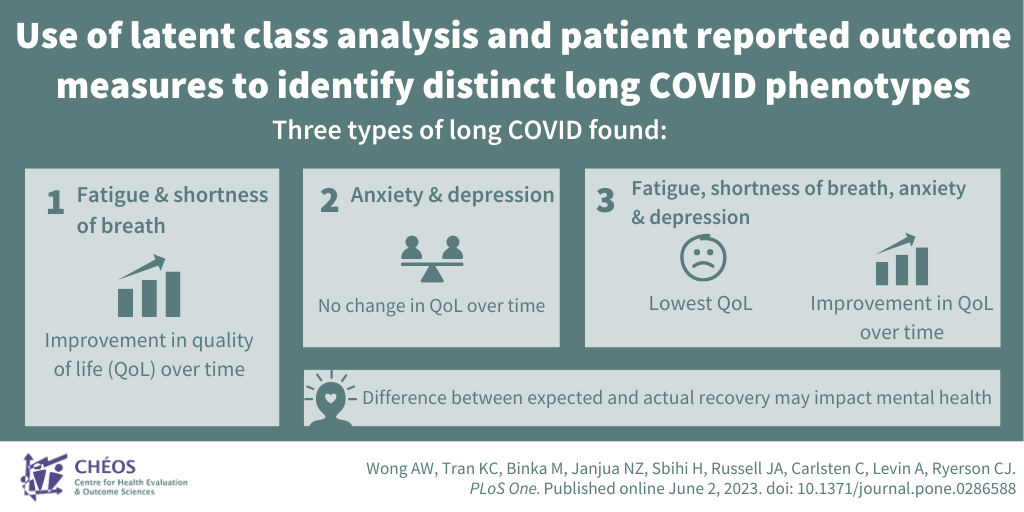
Patients’ symptoms can be grouped into three types of long COVID
Wong AW, Tran KC, Binka M, Janjua NZ, Sbihi H, Russell JA, Carlsten C, Levin A, Ryerson CJ. Use of latent class analysis and patient reported outcome measures to identify distinct long COVID phenotypes: A longitudinal cohort study. PLoS One. Published online June 2, 2023.
CHÉOS Scientists Drs. Karen Tran, Naveed Janjua, and Adeera Levin’s study aimed to identify and characterize different types of long COVID to see how they affect people’s health in the long term and help predict outcomes, personalize treatments, and understand the underlying causes. Using questionnaires to gather information about patients’ symptoms, the team found three types of long COVID: 1) fatigue and shortness of breath, 2) anxiety and depression, and 3) a combination of types 1 and 2. Patients with type 3 had significantly lower quality of life scores than other patients at 3 and 6 months after symptom onset. Over time, quality of life scores improved in patients with types 1 and 3, but not type 2. Types 2 and 3 (characterized by anxiety and depression) had a high proportion of people treated as outpatients. Among these outpatients, who are thought to experience mild disease, there may be a difference between their expected and actual recovery affecting their mental health. The study highlights the importance of identifying subpopulations of patients with long COVID who may have different outcomes and benefit from tailored therapeutic approaches.