The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
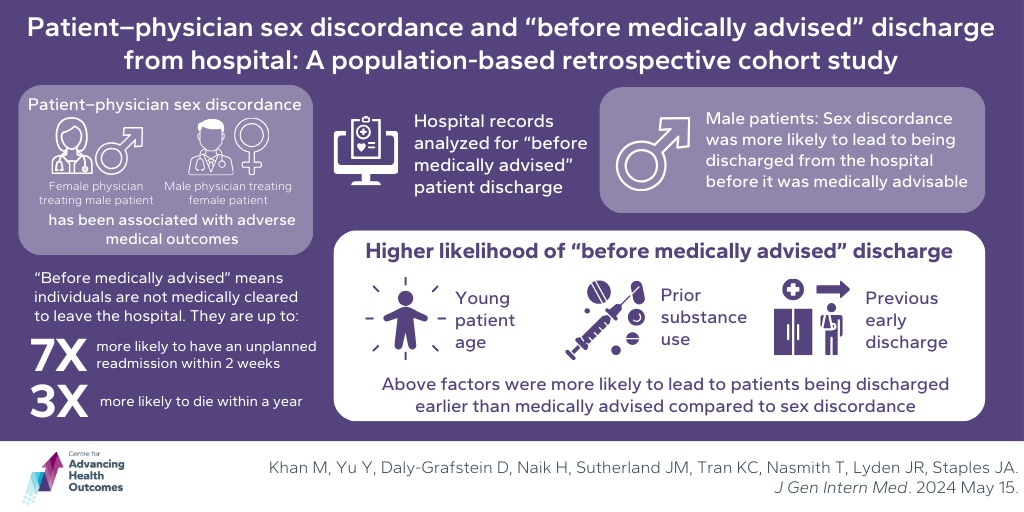
When people who use drugs seek support, formal support systems are preferred
Hayashi K, Rabu G, Cui Z, Klaire S, Homayra F, Milloy MJ, Nosyk B. Characterizing the use of healthcare access supports among people who use drugs in Vancouver, Canada, 2017 to 2020: A Cohort Study. Subst & Addict J. Published online May 28, 2024:29767342241249870. doi:10.1177/29767342241249870.
For people who use drugs (PWUD), ensuring fair access to health care can be achieved through various support systems. Formal supports include outreach workers and healthcare professionals and informal supports include friends and family. Few studies have looked at how often PWUD use formal and informal supports. Led by Dr. Bohdan Nosyk and supported by Advancing Health’s Fahmida Homayra, researchers evaluated what factors were linked to the use of formal and informal supports among PWUD. Data was analyzed from two studies of PWUD collected from 2017 to 2020. Statistical models were used to identify factors associated with using each type of support compared to no support. Out of 996 participants, 350 (35.1%) reported accessing supports in the past 6 months: 6.2% accessed informal supports, 14.1% accessed outreach workers, and 20.9% accessed health care professionals. Living with HIV, chronic pain, and avoiding health care due to past mistreatment were linked to increased engagement with health care professionals and outreach workers. It should be noted that those who were avoiding access to care due to mistreatment were more likely to receive support from outreach workers and peer navigators rather than healthcare professionals. Overall, the rate of accessing formal health care supports was relatively low among the participants. However, formal supports were more often accessed by PWUD with more health issues and those who faced discrimination in health care, highlighting the need to diversify care supports to help alleviate unmet healthcare needs.
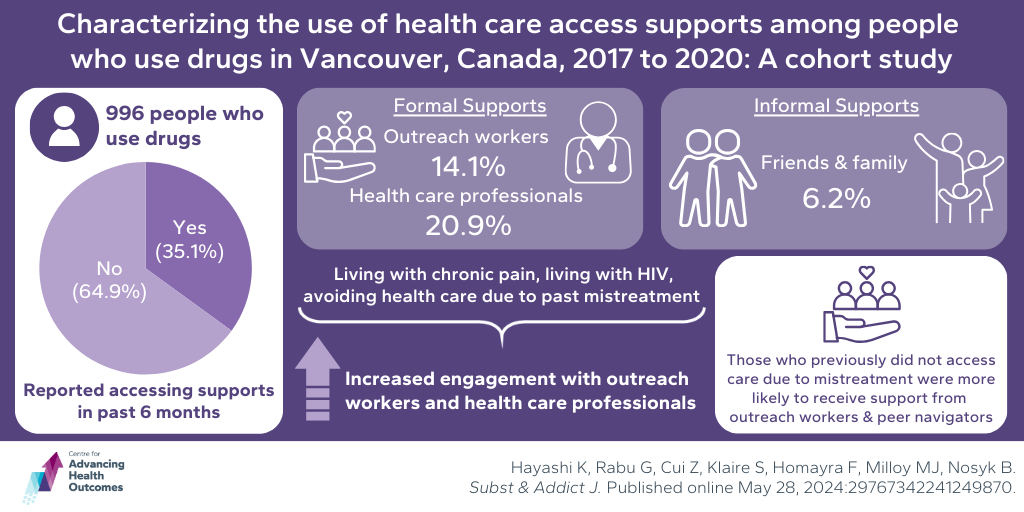
Post-COVID-19 condition lowers health-related quality of life
Naik H, Wilton J, Tran KC, Janjua NZ, Levin A, Zhang W. Long-term health-related quality of life in working-age COVID-19 survivors: A cross-sectional study. Am J Med. Published online May 23, 2024. doi:10.1016/j.amjmed.2024.05.016
Most adults aged 18–64 have been infected with SARS-CoV-2, with some developing post-COVID-19 condition, also called COVID. Post-COVID-19 condition has several symptoms including sleep problems, lightheadedness, brain fog, and depression or anxiety that can occur at least three months after infection and may last years. To better understand the impact of long COVID, Advancing Health Scientists Drs. Wei Zhang, Adeera Levin, Naveed Janjua, and Karen Tran conducted a cross-section survey of working-age individuals (18–64) to analyze health-related quality of life (HRQOL) over two years after COVID-19 infection. The study compared HRQOL among those who have post-COVID-19 condition, those who had recovered from it, and those who never had it. Out of 1,135 participants, 19.2% had current post-COVID-19 condition and 27.6% had recovered from it. Those who recovered had similar HRQOL to those who never had post-COVID-19 condition. Participants currently experiencing post-COVID-19 condition had a lower HRQOL and were more likely to report problems with mobility, self-care, pain or discomfort, and anxiety or depression. These results highlight the need for targeted health care interventions to improve HRQOL for adults with long-term post-COVID-19 condition.
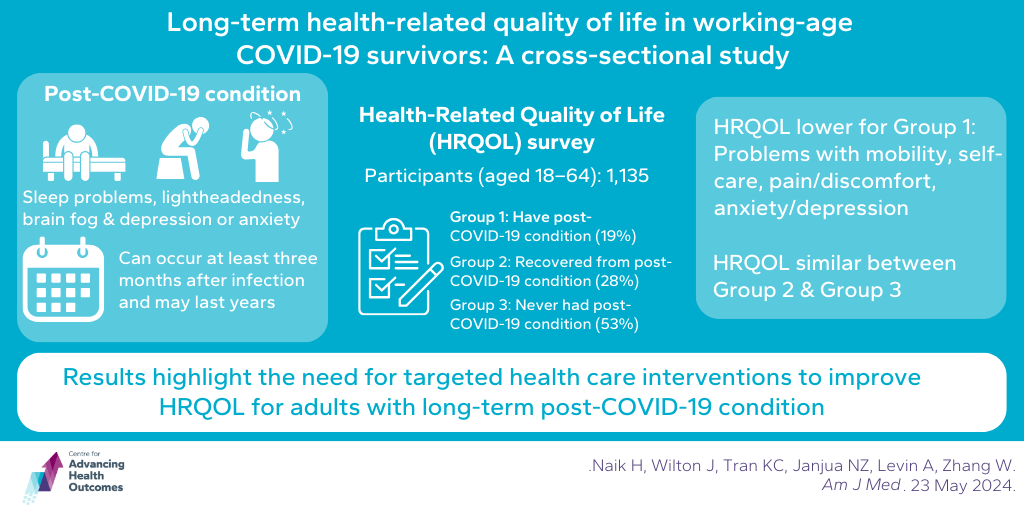
‘Before medically advised’ hospital discharge impacted more by age and substance use history than patient–physician sex discordance
Khan M, Yu Y, Daly-Grafstein D, Naik H, Sutherland JM, Tran KC, Nasmith T, Lyden JR, Staples JA. Patient–Physician Sex Discordance and “Before Medically Advised” Discharge from Hospital: A Population-Based Retrospective Cohort Study. J Gen Intern Med. Published online May 15, 2024:1-11. doi:10.1007/s11606-024-08697-8.
Patient–physician sex discordance (when the patient’s sex does not match the physician’s sex) has been associated with adverse medical outcomes including post-operative mortality and unplanned hospital readmission. Individuals departing hospital without medical clearance are up to seven times more likely to have an unplanned readmission within 2 weeks and up to three-fold more likely to die within a year. Research led by Advancing Health’s Dr. John Staples, supported by Drs. Karen Tran and Jason Sutherland, conducted a population-based retrospective cohort study to investigate whether the sex difference between patients and their physicians affects the likelihood of patient-initiated discharge from the hospital earlier than medically advised. Study data included all urgent (non-elective) admissions to any acute care hospital in BC with a discharge date between January 1, 2002 and March 31, 2017. Data were analyzed to compare the rates of early discharge between patients treated by physicians of the same sex and those treated by physicians of a different sex. The study found that among male patients, sex discordance was more likely to lead to being discharged from the hospital before it was medically advisable. However, younger patient age, prior substance use, and previous early discharge were more likely to lead to patients being discharged earlier than medically advised compared to sex discordance.