The Evidence Speaks Series is a recurring feature highlighting the latest in CHÉOS research. This series features summaries of select publications and is designed to keep media and the research community up to date with CHÉOS’ current research results in the health outcomes field.
To ensure this research is quick and easy to share, we are now providing social cards that you are free to save and use as you see fit.
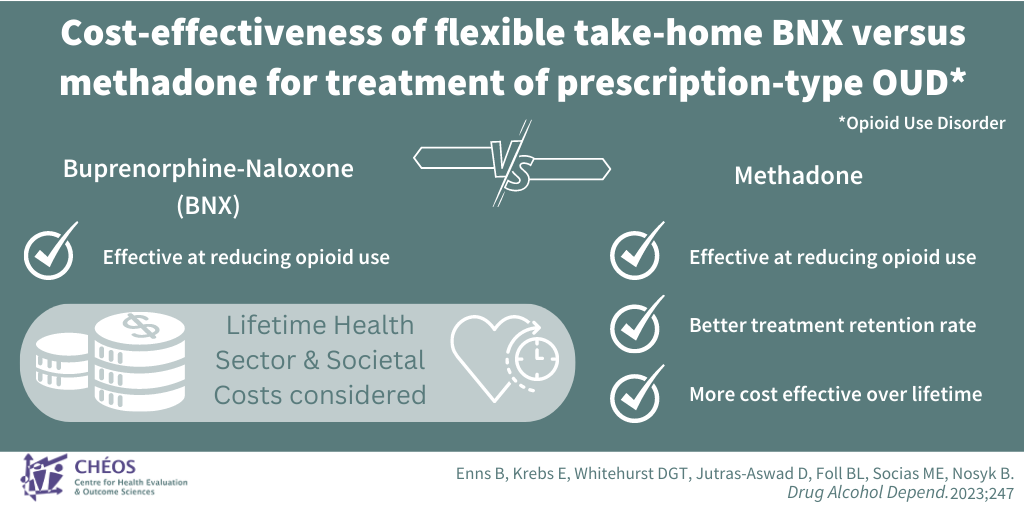
Buprenorphine-naloxone may not be a cost-effective treatment for OUD in the long run due to lower retention rates
Enns B, Krebs E, Whitehurst DGT, Jutras-Aswad D, Foll BL, Socias ME, Nosyk B. Cost-effectiveness of flexible take-home buprenorphine-naloxone versus methadone for treatment of prescription-type opioid use disorder. Drug Alcohol Depend. 2023 Jun 1;247:109893
CHÉOS Scientist Bohdan Nosyk, with staff members Benjamin Enns and Emanuel Krebs, led a team that compared the cost-effectiveness of two treatments for prescription-type opioid use disorder (OUD): flexible take-home buprenorphine-naloxone (BNX) and supervised methadone. The team used data from the OPTIMA trial, which found that BNX and methadone both effectively reduced illicit opioid use, and assessed the cost-effectiveness of these interventions. In the trial, more people stayed in the methadone treatment compared to the BNX treatment, and more individuals in the BNX group switched treatment. To assess cost–effectiveness, Dr. Nosyk and team considered health sector and societal cost perspectives, including costs for treatment, health resource use, and criminal activity. Assessing costs and benefits over a six-month period, the study revealed slight health benefits and cost savings associated with BNX. However, when evaluated over a lifetime, BNX was not cost-effective due to better treatment retention with methadone. These findings provide valuable insights for decision-making and treatment strategies for individuals with OUD.
—
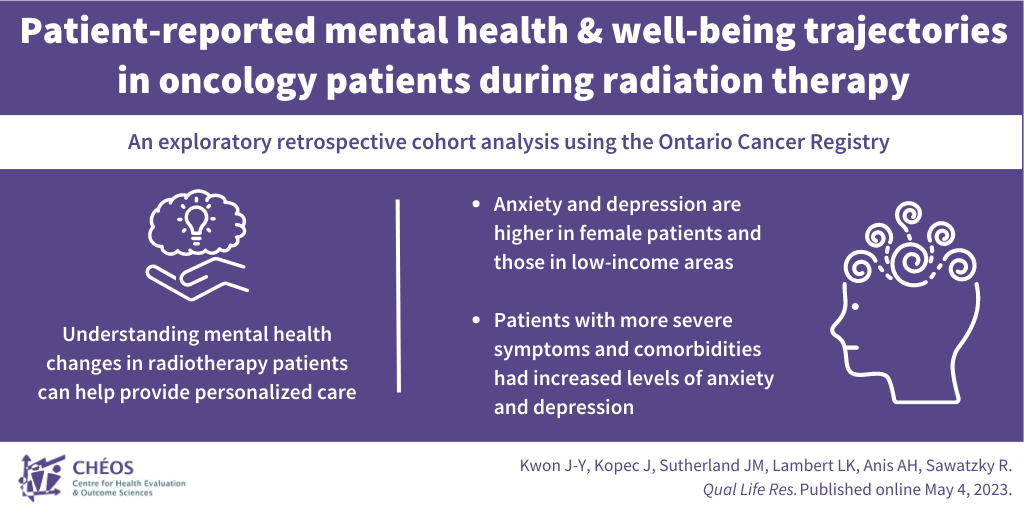
The emotions of cancer: Exploring the impact of socio-demographic factors on mental wellbeing in patients
Kwon J-Y, Kopec J, Sutherland JM, Lambert LK, Anis AH, Sawatzky R. Patient-reported mental health and well-being trajectories in oncology patients during radiation therapy: an exploratory retrospective cohort analysis using the Ontario Cancer Registry. Qual Life Res. Published online May 4, 2023.
CHÉOS Director Dr. Aslam Anis and CHÉOS Program Heads Drs. Jason Sutherland and Rick Sawatzky studied the emotional wellbeing of people receiving radiation therapy for cancer. They examined how factors like age, gender, where people live, and physical symptoms influenced changes in mental health during treatment. Overall, anxiety and depression decreased over time, indicating symptom improvement from initial oncology visit to >6 months later. Four subgroups of patients were identified, each with different mental health trajectories. One group had minimal symptoms throughout the treatment, while another initially experienced severe symptoms but improved over time. The remaining two groups showed diverse trajectories. Various socio-demographic and clinical factors were associated with how people felt, such as higher anxiety and depression reported by females and people living in low-income neighbourhoods. Understanding these different experiences can help clinicians provide better care and support, especially for those with the greatest mental health needs before and after radiation therapy.
—
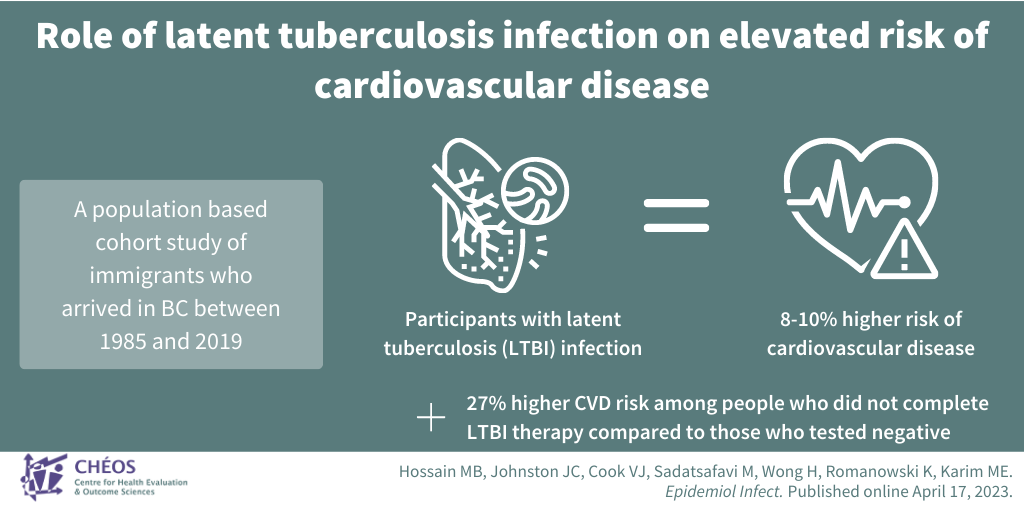
Despite not showing signs of infection, people with latent tuberculosis may be at increased risk of cardiovascular disease
Hossain MB, Johnston JC, Cook VJ, Sadatsafavi M, Wong H, Romanowski K, Karim ME. Role of latent tuberculosis infection on elevated risk of cardiovascular disease: a population-based cohort study of immigrants in British Columbia, Canada, 1985-2019. Epidemiol Infect. Published online April 17, 2023.
This research study aimed to investigate the association between latent tuberculosis infection (LTBI) and cardiovascular disease (CVD) among immigrants in B.C. Along with colleagues, Advancing Health’ Drs. Hubert Wong and Ehsan Karim used data from a cohort of immigrants who arrived in B.C. between 1985 and 2019. All participants had been tested for LTBI, which is a condition where a person carries tuberculosis bacteria but does not show symptoms of the disease. The team analyzed the data to determine if there was a higher risk of CVD among individuals with LTBI compared to those without LTBI. They also investigated whether completing LTBI therapy reduced the risk of CVD. The study concluded that LTBI is associated with an 8–10 per cent increased CVD risk in the province, with a higher risk associated with incomplete LTBI therapy and reduced risk when therapy is completed. This research contributes to the understanding of the relationship between LTBI and CVD in high-resource nations with low TB incidence.