The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
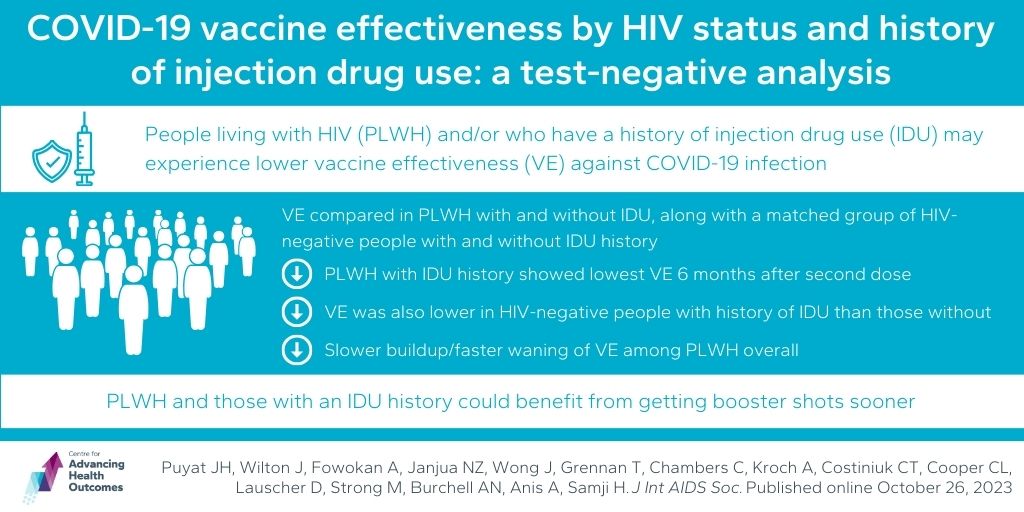
Early boosters for COVID-19 vaccine may benefit people living with HIV and with injected drug use history
Puyat JH, Wilton J, Fowokan A, Janjua NZ, Wong J, Grennan T, Chambers C, Kroch A, Costiniuk CT, Cooper CL, Lauscher D, Strong M, Burchell AN, Anis A, Samji H. COVID-19 vaccine effectiveness by HIV status and history of injection drug use: a test-negative analysis. J Int AIDS Soc. Published online October 26, 2023.
The Director of Advancing Health, Dr. Aslam Anis, along with scientists Drs. Joseph Puyat, Naveed Janjua, Troy Grennan, and Director of Grants Dr. Adeleke Fowokan, who undertook this study in his previous role as Epidemiologist at the BCCDC, studied how well COVID-19 vaccines work in people living with HIV (PLWH) and those with a history of injected drug use (IDU). Analyzing data from B.C., they found that PLWH with a history of injecting drugs may have less protection from COVID-19 vaccines. They compared vaccine effectiveness in PLWH with and without IDU history, along with a matched group of HIV-negative people. Results showed that overall vaccine effectiveness was lower in the first 6 months after the second dose for PLWH with IDU history compared to those without IDU history and HIV-negative individuals with or without IDU history. Vaccine effectiveness was also lower in the HIV-negative group with IDU history compared to those without. This suggests that PLWH and/or those with an IDU history might need booster shots sooner. However, it’s important to note that the study had limitations due to a small sample size.
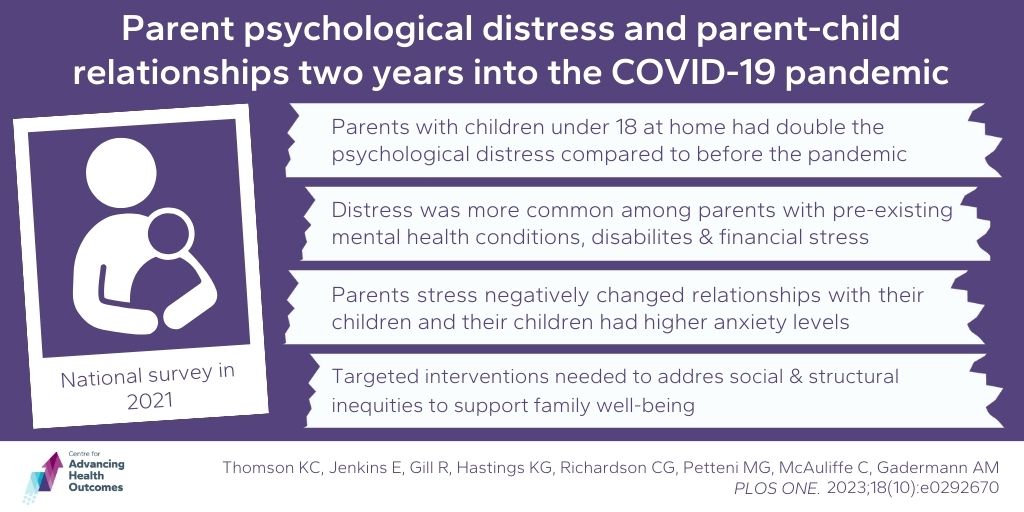
The ongoing impact of COVID-19 on family mental health
Thomson KC, Jenkins E, Gill R, Hastings KG, Richardson CG, Petteni MG, McAuliffe C, Gadermann AM. Parent psychological distress and parent-child relationships two years into the COVID-19 pandemic: Results from a Canadian cross-sectional study. PLOS ONE. 2023;18(10):e0292670.
Advancing Health scientists, Drs. Anne Gadermann and Chris Richardson, and trainee Monique Petteni, explored the lasting mental health challenges experienced by parents with children at home during the COVID-19 pandemic. Even though the pandemic affects mental health differently for everyone, parents were recognized early on as a group at heightened risk. Their study, based on a national survey in late 2021, showed that parents with children under 18 at home had almost double the psychological distress compared to before the pandemic. Distress was more common among parents with pre-existing mental health conditions, disabilities, and financial stress. They also found that parents feeling more stress had negative changes in how they interacted with their kids and noticed higher anxiety levels in their children. The team highlighted the challenges faced by parents and emphasized the need for targeted interventions to address social and structural inequities to support parental and family well-being.
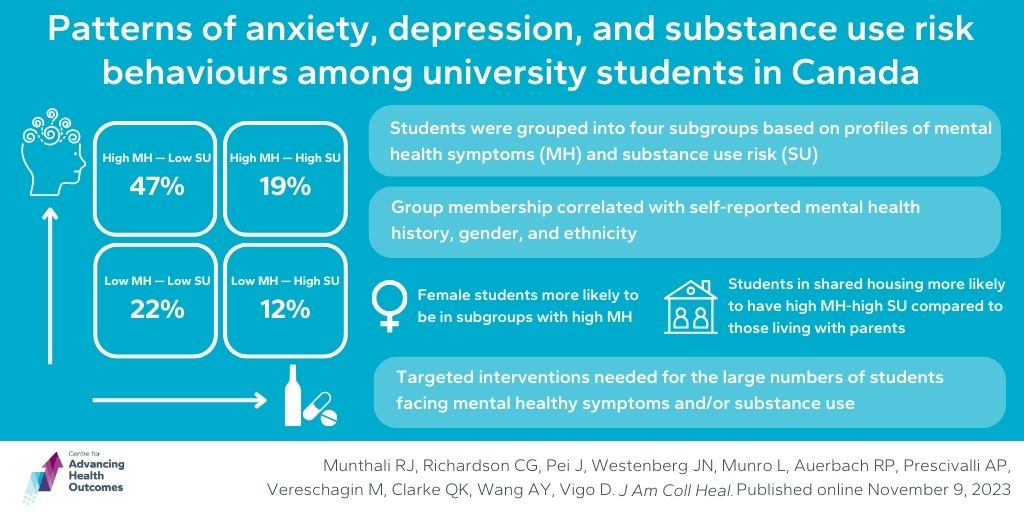
Early interventions may help student mental health and substance use
Munthali RJ, Richardson CG, Pei J, Westenberg JN, Munro L, Auerbach RP, Prescivalli AP, Vereschagin M, Clarke QK, Wang AY, Vigo D. Patterns of anxiety, depression, and substance use risk behaviors among university students in Canada. J Am Coll Heal. 2023.
Program Head of Psychosocial Epidemiology, Dr. Chris Richardson, and scientist, Dr. Daniel Vigo, collaborated on a study investigating anxiety, depression, and substance use risk behaviours among university students in Canada. Their aim was to identify unique profiles of mental health symptoms (MH) and substance use risk (SU) and explore how mental health history and socio-demographics predict a student’s profile. A weekly cross-sectional survey engaged almost 11,000 participants, revealing four student subgroups: High MH–Low SU (47%), Low MH–Low SU (22%), High MH–High SU (19%), and Low MH–High SU (12%). Group membership correlated with self-reported mental health history, gender, and ethnicity. Notably, female students tended to exhibit high MH, those in shared accommodation tended toward the high MH–high SU group compared to those living with parents, and Asian students were more prevalent in low SU groups than their white counterparts. The results confirm that a significant portion of students are facing mental health symptoms, substance use issues, or both, suggesting potential targeted early interventions based on gender, ethnicity, and mental health history.