The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
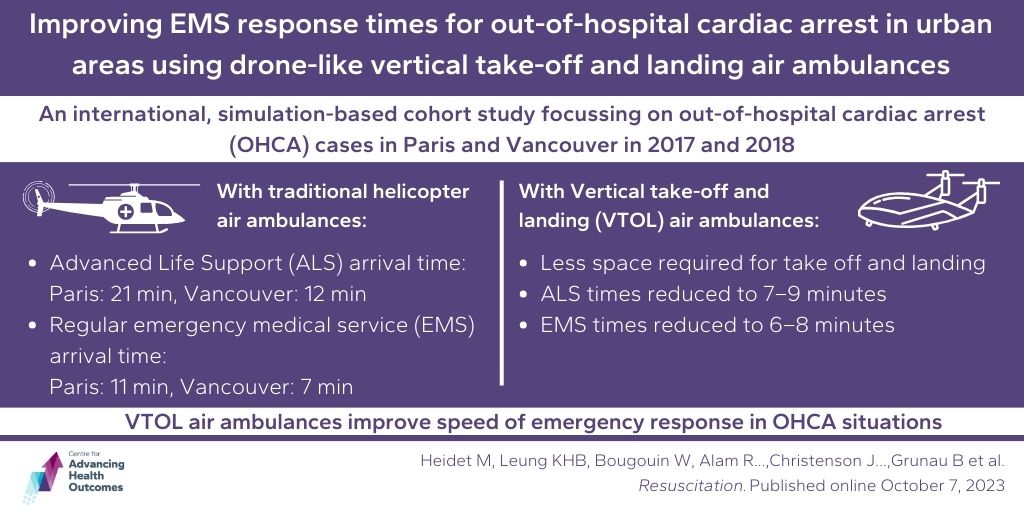
Incorporating multirotor-based air ambulances into out-of-hospital cardiac arrest response could improve response times for patients
Heidet M, Leung KHB, Bougouin W, Alam R, Frattini B, Liang D, Jost D, Canon V, Deakin J, Hubert H, Christenson J, Vivien B, Chan T, Cariou A, Dumas F, Jouven X, Marijon E, Bennington S, Travers S, Souihi S, Mermet E, Freyssenge J, Arrouy L, Lecarpentier E, Derkenne C, Grunau B. Improving EMS response times for out-of-hospital cardiac arrest in urban areas using drone-like vertical take-off and landing air ambulances: an international, simulation-based cohort study. Resuscitation. Published online October 7, 2023.
A team including Advancing Health Scientists Drs. Jim Christenson and Brian Grunau have been looking at how using special aircraft called vertical take-off and landing (VTOL) air ambulances could help save lives during out-of-hospital cardiac arrests (OHCA) in cities like Paris and Vancouver. These VTOL aircraft can carry two emergency medical services (EMS) workers and one patient, and can take off and land in small spaces (20×30 ft), making it easier to reach crowded city areas that regular helicopters can’t.
The study focused on OHCA cases from January 2017 to December 2018 and looked at how quickly help arrived. In Greater Paris, it took about 21 minutes for advanced life support (ALS) teams to get to OHCA cases, and 12 minutes in Metro Vancouver. Regular EMS teams took 11 minutes and 7 minutes to arrive, respectively. Unfortunately, chance of survival decreases between 7% and 10% for each minute that elapses between the cardiac arrest and initiation of CPR.
When they added 1–2 VTOL air ambulances into the response using a simulation model using data from the manufacturer, the response times got much faster. ALS times were reduced to 7–9 minutes and regular EMS teams to 6–8 minutes in both locations. By integrating VTOL, up to 96% of OHCA cases in Paris and 94% in Vancouver could have ALS units arrive within 10 minutes of the emergency call, an improvement from historical response rates of 2% and 36%. This research shows that using VTOL air ambulances could really speed up how quickly help gets to people during OHCA emergencies.
Enhancing health and well-being during surgical wait times could improve waitlist management
Wiseman SM, Sutherland JM. Improving the quality of care of Canadians waiting for elective surgery: an important health care priority. Can J Surg. 2023;66(5):E474-E475.
Surgical wait lists are a big problem for patients, their families, doctors, the health care system, and governments. Published in the Canadian Journal of Surgery, Advancing Health’s Dr. Jason Sutherland and Dr. Sam Wiseman, Director of Research in the Department of Surgery at Providence Health Care, have offered potential solutions.
First, they advise implementing patient-centered triaging methods when prioritizing surgeries. This approach considers factors like how much pain someone is in or how much their health will improve, rather than just how long they’ve been waiting. They also suggest having a multidisciplinary team of experts to make these priority decisions.
Secondly, they recommend providing mental health support and exercise assistance to patients during their waiting period. Prolonged wait times for surgery can result in disease progression, heightened anxiety and depression, mental health issues, and worsened patient outcomes. Given that waiting times are unlikely to decrease quickly, looking after the health and well-being of patients in the queue can optimize surgical outcomes, while also streamlining the management of surgical wait lists.
Together with other evidence-based solutions and support services, Drs. Sutherland and Wiseman suggest that these changes can help to reduce complexity, improve quality, and reduce disparities, ultimately benefiting the welfare of people in Canada.

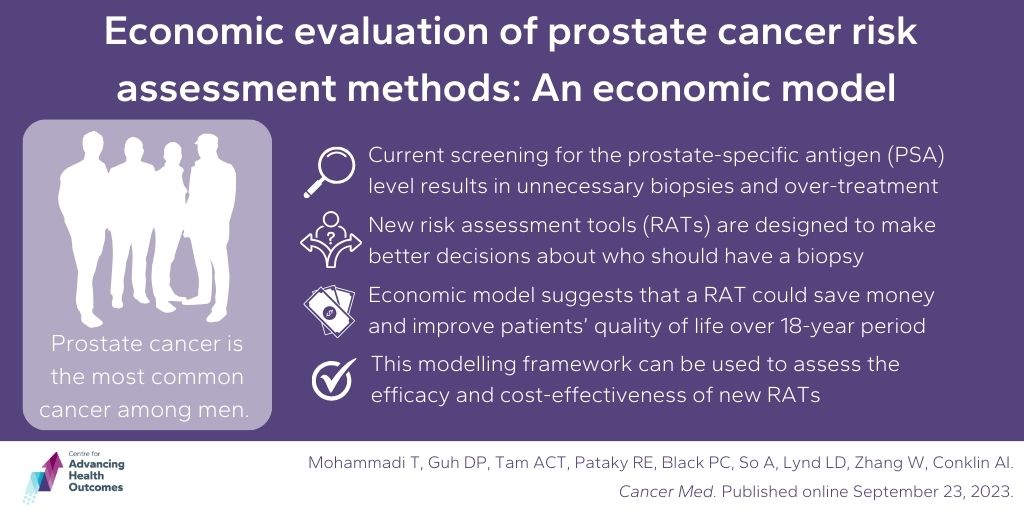
New Risk Assessment Tools (RAT) for prostate cancer could improve patients’ quality of life and save money
Mohammadi T, Guh DP, Tam ACT, Pataky RE, Black PC, So A, Lynd LD, Zhang W, Conklin AI. Economic evaluation of prostate cancer risk assessment methods: A cost-effectiveness analysis using population data. Cancer Med. Published online September 23, 2023.
Advancing Health Scientists, Drs. Larry Lynd, Wei Zhang and Annalijn Conklin, are working to improve how we screen for prostate cancer, the most common cancer among men. Currently, a test for the prostate-specific antigen (PSA) level is used to decide if a biopsy is necessary. However, this test isn’t very accurate, leading to unnecessary biopsies and overtreatment which can be risky to patients and costly to the health care system.
New risk assessment tools (RATs) aim to make better decisions about who should have a biopsy. The team designed a modeling framework to assess the efficacy and cost effectiveness of new RATs.
By using data from existing studies, the team simulated the use of a novel RAT in a cohort of patients and found that incorporating an accurate tool in the initial diagnosis of prostate cancer would not only save money, but also improve patients’ quality of life over an 18-year period — saving $44 per patient and increasing quality-adjusted life years (QALY) by 0.00253. Moreover, when they set a cost-effectiveness threshold of $50,000 per QALY, there was a 73% chance that using the RAT was more cost-effective compared to the current standard of care.
However, the outcomes were sensitive to RAT accuracy, their cost, the detection rate of high-grade prostate cancer, cancer prevalence, and assumptions about survival of undetected prostate cancer. This general model can be used to analyze the cost-effectiveness of any novel RAT and suggests that a more precise test for guiding biopsy decisions could be a wise investment in improving health care.