The Evidence Speaks Series is a recurring feature highlighting the latest in Advancing Health research. This series features summaries of select publications and is designed to keep media and the research community up to date with the Centre’s current research results in the health outcomes field.
To ensure this research is quick and easy to share, you are welcome to save the social cards and use as you see fit.
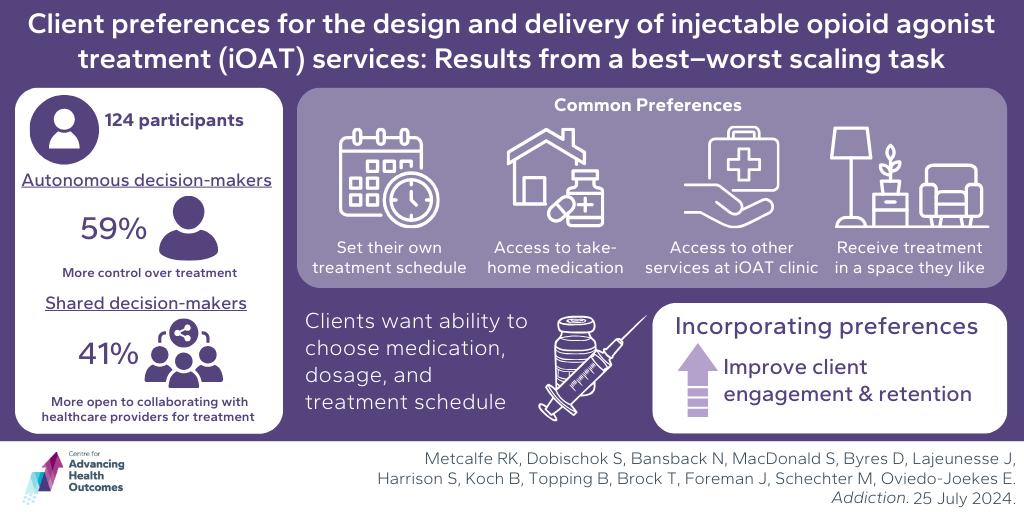
iOAT clients want more autonomy in their treatment
Metcalfe RK, Dobischok S, Bansback N, MacDonald S, Byres D, Lajeunesse J, Harrison S, Koch B, Topping B, Brock T, Foreman J, Schechter M, Oviedo-Joekes E. Client preferences for the design and delivery of injectable opioid agonist treatment services: Results from a best–worst scaling task. Addiction. Published online July 25, 2024. doi:10.1111/add.16620
Despite recommendations and evidence indicating that individualized care improves engagement, retention, and outcomes for people with opioid use disorder (OUD), system-level requirements often dictate how injectable opioid agonist treatment (iOAT) can be delivered, preventing iOAT programs from effectively providing person-centered care. A study led by Advancing Health’s Dr. Rebecca Metcalfe, with Drs. Nick Bansback, Martin Schechter, and Eugenia Oviedo-Joekes, explored the preferences of people receiving iOAT in Vancouver, Canada. There were 124 participants surveyed, most of whom were current iOAT clients. By analyzing responses using the best-worst scaling survey method, the researchers identified two main groups of clients with different preferences: 1) autonomous decision-makers and 2) shared decision-makers. Autonomous decision-makers preferred to have more control over their treatment decisions and shared decision-makers were more open to collaborating with health care providers on treatment decisions. Despite these differences, both groups shared several common preferences including access to take-home medication, ability to set their own treatment schedule, receiving treatment in a space they like, and having access to other services, such as primary care and counselling, at the iOAT clinic. The study found that, overall, iOAT clients in Vancouver desire more autonomy in their treatment, most notably their medication type and dosage, as well as their treatment schedule. These findings highlight the importance of considering client preferences in designing and delivering iOAT services with the goal of improving client engagement, retention, and outcomes for people with OUD.
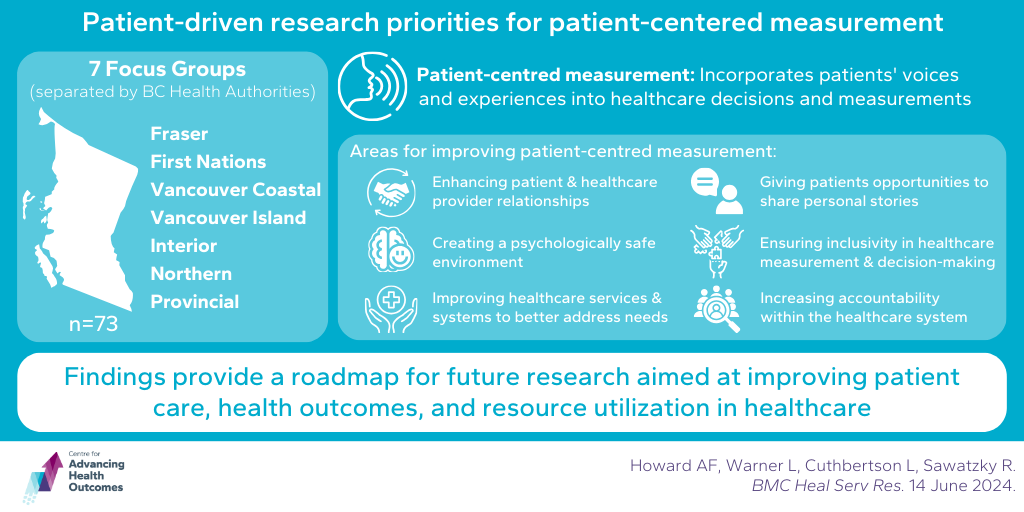
Patients highlight several areas for improving patient-centered measurement
Howard AF, Warner L, Cuthbertson L, Sawatzky R. Patient-driven research priorities for patient-centered measurement. BMC Heal Serv Res. 2024;24(1):735. doi:10.1186/s12913-024-11182-x
Patient-reported outcome and experience measures are tools used to capture the impact of illness on a person’s health and quality of life, and their experiences of care. Advancing Health’s Dr. Rick Sawatzky and his team investigated how to improve patient-centred measurement in health care by focusing on patients’ perspectives. The researchers held seven focus groups across the province, involving 73 patients. They analyzed the discussions to identify key priorities for advancing patient-centred measurement research and practice. The study found that patients want their individual healthcare needs and priorities to be at the forefront of all health care interactions. They highlighted six main areas for improving patient-centred measurement: 1) enhancing relationships between patients and health care providers; 2) giving patients opportunities to share their personal stories; 3) ensuring inclusivity in health care measurement and decision-making; 4) creating a psychologically safe environment for patients; 5) improving health care services and systems to better address patient needs; and 6) bolstering health care system accountability. These findings provide a roadmap for future research aimed at improving patient care, health outcomes, and resource utilization in health care.
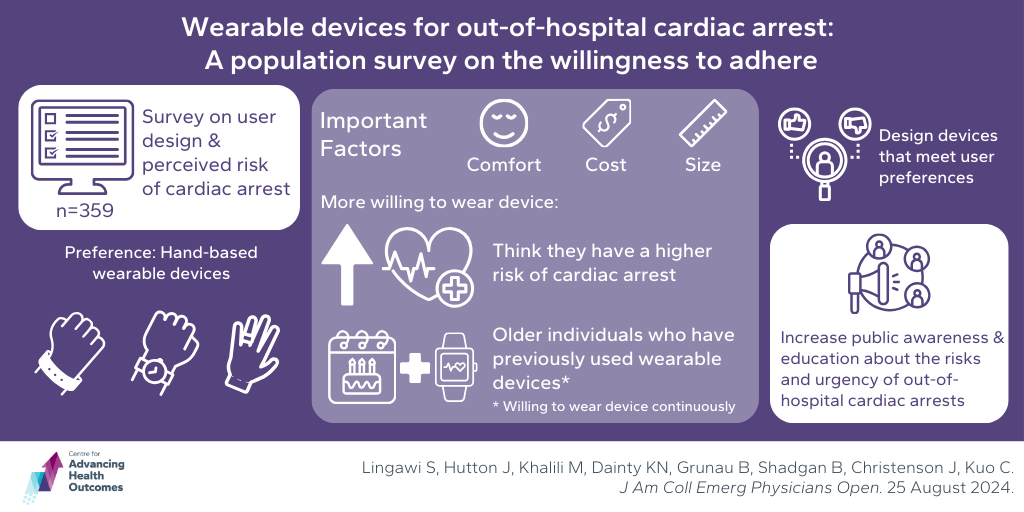
Design, awareness, and education impact willingness to wear early OHCA detection device
Lingawi S, Hutton J, Khalili M, Dainty KN, Grunau B, Shadgan B, Christenson J, Kuo C. Wearable devices for out-of-hospital cardiac arrest: A population survey on the willingness to adhere. J Am Coll Emerg Physicians Open. 2024;5(5):e13268. doi:10.1002/emp2.13268
When an out-of-hospital cardiac arrest (OHCA) occurs, the first step in the chain of survival is detection: each minute without medical care significantly decreases the chances of survival. However, the majority of OHCAs are not observed by a witness, which warrants the need for wearable devices that could detect an OHCA and alert emergency services. A study with Advancing Health Trainees Jacob Hutton and Dr. Mahsa Khalili, supported by Drs. Brian Grunau and Jim Christenson, explored people’s attitudes towards wearing such devices. A survey with 359 respondents found that people preferred hand-based devices, such as wristbands, watches, and rings, and important factors to consider were comfort, cost, and device size. People were more willing to wear the devices if they thought they had a higher risk of experiencing cardiac arrest. Older individuals who had previously used wearable devices were most willing to wear these devices continuously, even at a low baseline risk. The authors also concluded that optimizing willingness is not just a matter of adjusting for user preferences, but also increasing the understanding of urgency regarding OHCA through awareness and education.